These frequently asked questions are updated regularly. Here you will find answers to a range of common questions we are often asked about our organisation and the services we deliver.
We are part of NHS Resolution. We support the resolution of performance concerns about individual doctors, dentists and pharmacists.
Our assessment services are aimed at clarifying and understanding the performance of individual practitioners and providing healthcare organisations and practitioners with a sound basis upon which to bring the case towards a resolution. Assessments are not an end point in themselves, but are a valuable tool to support the effective management of cases locally.
Assessments are not an investigation of the incidents which may have led to the referral to us.
The employing/contracting organisation will normally have asked for, and received, advice from us on how to manage the concern with the practitioner. As part of that process they will have been told about the assessments and other interventions available and will have then decided to request an assessment.
Requests for assessment are considered by our Intervention Consideration Group in line with our published policy and a formal decision to accept or decline the request will then be issued. We need the agreement of both the employing/contracting organisation and the practitioner before we can consider such a request.
If the request for an assessment is approved then we draw up an ‘agreement to assessment’ which sets out the purpose of the assessment and explains how the assessment will be carried out. It also sets out the responsibilities of Practitioner Performance Advice, the practitioner and the employing/contracting organisation with regard to the assessment.
We will not be able to proceed with the assessment until the agreement to assessment has been signed by both the practitioner and employing/contracting organisation to confirm their commitment to the process.
Clinical Performance Assessment
The purpose of a Clinical Performance Assessment is to provide an independent view on the clinical performance of the practitioner, identifying both satisfactory practice and any areas of poor practice.
The assessment is intended to provide information to assist the referring organisation in decisions about the next steps in their management of the case.
Behavioural Assessment
A Behavioural Assessment provides an independent view on the behavioural characteristics of the practitioner, including any areas which require consideration.
The assessment is intended to provide information to assist the referring organisation in decisions about the next steps in their management of the case.
Clinical Performance Assessment
The assessment is carried out through a clinical assessment visit by a trained team of two clinical assessors and a Senior Assessment and Remediation Manager. It includes:
- Clinical record review: of a sample of patient records.
- Direct observation of practice: the practitioner’s normal clinical work.
- Case-based assessment: exploring clinical reasoning and decision-making about the practitioner’s own cases.
Clinical assessors will have relevant clinical experience in the practitioner’s speciality, be familiar with the standards relating to their clinical specialty and be able to apply them to assess the performance of a peer. We also ensure that they are in good standing with the relevant professional bodies and regulators.
Behavioural Assessment
The assessment includes:
- The practitioner completing three online psychometric questionnaires (the Revised NEO Personality Inventory, the Hogan Development Survey and the Motives, Values, Preferences Inventory).
- The practitioner attending an interview with a behavioural assessor (an occupational psychologist), during which the assessor asks a range of questions about the practitioner’s work, including: what they do in their job, which aspects they enjoy most and least, how they approach the different aspects and demands of their role etc. The interview is conducted remotely, via videoconference, in two sessions of around two to three hours each. After the first session, the psychologist usually gives initial feedback to the practitioner.
Practitioner Performance Advice produces an assessment report which will provide the employing/contracting organisation with clear findings and conclusions about the practitioner’s level of performance (for clinical practice assessments) and with an independent view on the behavioural characteristics of the practitioner, including any areas which require consideration (behavioural assessments).
We are available to offer advice and recommendations to employing/contracting organisations on next steps after the assessment. This can include asking our Professional Support and Remediation service to prepare an action plan to support a practitioner’s return to safe and effective practice (for clinical performance assessments) and to help consideration of behavioural issues (for behavioural assessments).
We recognise that where questions have been raised about a practitioner’s work, this can be a very stressful experience for the individual concerned. We are committed to ensuring the services we offer and the way we deliver our services are sensitive to the impact on the individual about whom questions have been raised.
We always recommend that practitioners access appropriate and timely professional support through their defence organisation or other representative body. We would also encourage practitioners to draw on personal support that is available to them, for example, through friends or family.
The practitioner’s General Practitioner can also be an important source of support.
It also worth remembering that support is available through the healthcare organisation, for example, through its local occupational health and counselling services. More avenues of support may be available locally or accessed through the relevant Royal College.
Our website also contains details of organisations that may be of use to practitioners – please see the link below:
Each case has an assigned Case Adviser who is available to speak to the practitioner and to the employing/contracting organisation about any matters relating to the case and to answer any questions about our services. If you wish to speak to the Case Adviser, please call 020 7811 2600 or email nhsr.advice@nhs.net.
If you have any questions about the assessment process itself, you can email: nhsr.assessment@nhs.net.
For further information on our assessments, please click on the following links:
Please refer to our Covid-19 Vaccinations NHS Staff Indemnity – FAQs, which are available from our Covid-19 Vaccinations webpage.
The Clinical Negligence Scheme for Trusts (CNST) is a scheme for handling clinical negligence claims against NHS trusts.
Individual member contribution levels are influenced by a range of factors, including the type of trust, the specialties it provides and the number of “whole time equivalent” clinical staff it employs. Claims history is also taken into account meaning that members with fewer, less costly claims pay less in contributions.
When a claim is made against a member of CNST, the NHS body remains the legal defendant. However, NHS Resolution takes over full responsibility for handling the claim and meeting the associated costs.
The CNST covers all clinical claims occurring on or after 1 April 1995. If an NHS Body joined later than this date, then they are covered from the date they join the scheme.
Yes. The administration of injectable contraceptives is an activity connected to the provision of primary medical services under a GP contract and hence in scope of CNSGP.
NHS Resolution can confirm that Physician Associates (PAs) working for general practice who are carrying out activities connected to delivering NHS primary medical services on behalf of the provider under a primary care contract in England, namely one which falls within Part 4 of the NHS Act 2006 (GMS, PMS and APMS arrangements), will be indemnified under the Clinical Negligence Scheme for General Practice (CNSGP) for clinical negligence liabilities arising from incidents that occurred on or after 1 April 2019. This is because CNSGP provides indemnity cover for all GPs and staff working under an NHS GP contract in England in respect of liabilities in clinical negligence.
This indemnity extends to activities carried out by PAs which are connected to the delivery of other NHS services provided by general practice and known as ‘Ancillary Health Services’ where these services fall within the relevant definition in regulation 2 of the CNSGP Regulations.
GP partners/GP principals and other clinical staff responsible for the supervision of PAs within general practice can also be reassured that they will be indemnified as above, in respect of incidents involving PAs which result in a clinical negligence claim that is brought against the partners/principals or practice, or where their role in the incident involving the actions of a PA and resulting in a claim was limited to supervision of the PA.
Please note that indemnity under CNSGP is for liabilities in clinical negligence only. The scheme does not provide indemnity cover for non-clinical matters, advice or professional (regulatory) matters. We would recommend indemnity cover be obtained from an MDO or other indemnity provider for those matters outside the scope of CNSGP, such as non-NHS work.
For any enquiries please contact:nhsr.cnsgp@nhs.net
You may also find the following resources helpful:
CNSGP (GPI) scheme scope document
GPI reporting flowchart
Yes. The Enhanced Service Specification: Seasonal influenza vaccination programme 2025/26 enabled practices to offer their frontline patient-facing staff working in general practice a flu vaccination, effective from 1 October 2025.
This covers frontline patient-facing staff and locum GPs who are registered with the GP practice as well as those who are not registered with the GP practice but who elect to receive their vaccination from the GP practice (therefore including peer to peer vaccinations).
As the service is offered and provided under the terms of the seasonal influenza vaccination enhanced service specification and therefore under a primary medical services contract (GMS, PMS, APMS or Schedule 2L provisions under an NHS Standard Contract) the activity falls within the scope of the Clinical Negligence Scheme for General Practice (CNSGP)
For further information regarding the 2025/26 seasonal influenza vaccination programme, please refer to the following guidance published by NHS England:
Enhanced service specification: seasonal influenza vaccination programme 2025/26: General Practice Enhanced Service Specification Seasonal influenza vaccination programme 2025/26
Additional guidance on the recording of flu vaccination events: NHS England » General Practice Seasonal Influenza Vaccination Programme Additional Guidance
In the first instance you should speak with your MDO. It is important to do this as soon as you become aware of your involvement or potential involvement in an inquest, so they can provide you with as much support as possible. Late notification may limit the extent of assistance that can be provided by your MDO.
NHS Resolution will only become involved if a claim is intimated or likely. If you believe that being involved in an inquest is linked to an incident that could result in a potential claim under the Clinical Negligence Scheme for General Practice or whether a matter should be reported, please contact NHS Resolution by:
1. Email – nhsr.cnsgpnotification@nhs.net
– setting out the basis of your enquiry and we will either respond by email or telephone to discuss the issue further. Do not send any documents via email as they may contain patient sensitive data. Do not include any patient sensitive data in your email.
2. Telephone – call our Claims Helpline 0800 030 6798 at any time; 24 hours a day, 365 day a year to speak to a legal advisor about any clinical negligence claims covered by CNSGP.
For guidance and background NHS Resolution has made three short films providing information on what to expect when called to an inquest. They can be viewed here.
Please refer to our Covid-19 Vaccinations NHS Staff Indemnity – FAQs, which are available from our Covid-19 Vaccinations webpage.
There is no blanket requirement for you to notify NHS Resolution of conditions placed on your licence to practice. We may however request you to provide this information where you are involved in a claim notified to us and these details are reasonably required for the purposes of enabling NHS Resolution to effectively manage the claim on your behalf in accordance with the scheme rules.
In the event details of practice conditions are provided to NHS Resolution where we have not requested this information, we will respond to make it clear that we do not need to be notified and the information will be deleted.
If you are required by your MDO or other indemnifier to report such matters, you should continue to do so.
All providers of NHS primary medical services are covered under CNSGP, including out of hours providers. The scheme extends to all GPs and others working for general practice who are carrying out activities in connection with the delivery of primary medical services – including salaried GPs, locums, students and trainees, nurses, clinical pharmacists, agency workers and other practice staff.
In addition to NHS primary medical services, any other NHS services provided by general practice are also covered under CNSGP (namely, NHS activities carried out by or for a provider whose principal activity is to provide NHS primary medical services). These ‘other’ NHS services are referred to in the regulations that establish CNSGP[1] as “ancillary health services”. This means general practices are covered for all of their NHS services, including local authority commissioned public health services.
The place at which activities are carried out, the status of the person carrying out the activity, the form of the entity responsible for the provision of the NHS services in question and the individual circumstances of the patient concerned are not relevant to the scope of CNSGP. The question is whether the services provided are NHS primary medical services, and where they are not NHS primary medical services, whether they are NHS services provided by general practice [namely, by a provider whose principal activity is to provide NHS primary medical services]. This means that different kinds of organisations are covered under the scheme for activities they carry out which are in scope of the scheme.
Claims made against GP practices or other organisations providing NHS primary medical services or ancillary health services are covered under the scheme. This includes claims made in respect of liabilities that arise as a consequence of the acts or omissions of employees and others engaged to carry out activities connected to the provision of such services.
This scheme scope table outlines types of work carried out by general practice staff and whether or not it is covered by CNSGP.
The scheme applies to any liability in tort (civil wrongdoings which include clinical negligence) that arises as a consequence of a breach of a duty of care owed by a GP contractor[2] or GP sub-contractor[3] to a third party in connection with the provision of primary medical services or ancillary health services where –
(a) An act, or omission, on the part of the GP contractor/sub-contractor (or any employee or other person engaged by them) results in personal injury or loss to the third party;
(b) The act, or omission, is in connection with the diagnosis of an illness or the provision of care or treatment to the third party; and
(c) The act or omission occurs on or after 1 April 2019.
[1] The National Health Service (Clinical Negligence Scheme for General Practice) Regulations 2019.
[2] A GP contractor is a person or organisation who holds a general medical services (GMS), personal medical services (PMS) or alternative provider medical services (APMS) contract or agreement made under Part 4 of the National Health Service Act 2006 – i.e. GP contracts.
[3] A GP sub-contractor is a person or organisation that provides primary medical services under a sub-contract with a GP contractor (i.e. a primary medical services sub-contractor. It also includes a person providing ancillary health services under a sub-contract with a GP contractor or a primary medical services sub-contractor.
If the activity consists of, or is in connection with, the provision of primary medical services under a general medical services (GMS), personal medical services (PMS) or alternative provider medical services (APMS) contract, or APMS contract under schedule 2L of NHS Standard Contracts, any clinical negligence liability incurred arising from that activity is covered under the scheme.
If the activity is not being delivered under one of the above contracts, it is covered by the scheme if the answers to all the following questions are affirmative:
- Is it an activity that consists of, or is in connection with, the provision of NHS services?
- Are those NHS services being carried out by or for a provider whose principal activity is to provide NHS primary medical services (i.e. the NHS services are provided as part of general practice) or under a sub-contracting arrangement with such a provider?
- Is the activity in question connected to the diagnosis, care or treatment of a patient?
These claims will not be covered by the CNSGP as they relate to care, treatment or diagnosis before the scheme came into operation. They will need to be reported to your medical defence organisation (MDO) or other indemnity provider. Please note that your indemnity provider will be NHS Resolution where terms have been agreed with MDOs in relation to indemnity provision for their GP members under the Existing Liabilities Scheme for General Practice (ELSGP). The ELSGP currently only covers historical liabilities for those who were members of the Medical and Dental Defence Union of Scotland (MDDUS) and the Medical Protection Society (MPS) at the time of the incident in respect of which a claim is made. For further information on ELSGP and how to make a claim under it, please see here.
The part of the claim referring to the treatment and/or care occurring before 1 April 2019 will be dealt with by the relevant indemnity or insurance provider. Please note that your indemnity provider will be NHS Resolution where terms have been agreed with MDOs in relation to indemnity provision for their GP members under the Existing Liabilities Scheme for General Practice (ELSGP). The ELSGP currently only covers historical liabilities for those who were members of the Medical and Dental Defence Union of Scotland (MDDUS) and the Medical Protection Society (MPS) at the time of the incident in respect of which a claim is made. For further information on ELSGP and how to make a claim under it, please see here. CNSGP will cover the element of the treatment and/or care that occurred after 1 April 2019.
All activities relating to the diagnosis of an illness or the provision of care or treatment and carried out under a general medical services (GMS), primary medical services (PMS) or alternative provider medical services (APMS) contract are covered by CNSGP. If the provision of primary medical services under such contracts is your principal activity, all of your NHS work is covered, as the activities fall within scope of the scheme.
Any activities relating to your private practice are not covered and you need to purchase suitable indemnity or insurance to cover such work.
If you are employed by the trust, or your contract with the trust states that the trust accepts liability for your acts/omissions, then you are likely to be covered by the Clinical Negligence Scheme for Trusts (CNST). If the services you provide for the trust are part of the NHS services provided by general practice, then you are likely to be covered by CNSGP.
Any treatment or care you provide to your patients under a GMS, PMS or APMS contract is covered by CNSGP. Any treatment you provide privately (e.g. a patient who pays you for services not provided as part of the NHS) is not covered. It is possible, then, that some of the services you offer to an individual patient are covered by CNSGP and some are not (and therefore you require additional indemnity from another provider for services not covered under CNSGP).
A key challenge for general practice has been to find a solution to the growing cost of indemnity cover. Introducing a state scheme removes the risk of rising indemnity costs from individual GPs and other healthcare practitioners (e.g. nurses and pharmacists) working in general practice. People working in general practice do not need to pay to be covered by CNSGP. CNSGP provides fully comprehensive cover for all claims within its scope.
You don’t need to do anything or to become a member. From 1 April 2019, all GPs and others working in general practice are automatically covered under CNSGP for liabilities arising from the provision of NHS primary medical services and ancillary health services as part of the NHS for England. You do not need to pay a subscription. The costs of the scheme are met centrally.
The only ongoing costs for GPs and other healthcare professionals working in general practice relate to any indemnity arrangement to ensure you are adequately protected for those activities which are not covered under CNSGP, and any run off cover that is required in relation to incidents that occurred prior to 1 April 2019. Please familiarise yourself with the terms of the Existing Liabilities Scheme for General Practice (ELSGP), which came into effect on 6 April 2020, when considering whether or not to purchase run-off cover.
We have published separate guidance on when and how to report a claim. The guidance can be found here: CNSGP – When and how to report a claim.
Activities not covered by CNSGP include:
- Any healthcare delivered otherwise than through the NHS or local authority funded contracts for NHS public health services. This includes privately funded work undertaken by GPs and other primary care health professionals working in GP practices;
- Other non-NHS activities such as reports and medicals undertaken by GPs for other departmental bodies and insurance work, which falls outside of essential services;
- NHS primary care dentistry and private practice dentistry, other forms of privately-funded primary healthcare, community pharmacy and optometry;
- Medico-legal services (other than those directly relating to clinical negligence claims), such as representation at inquests or in relation to professional regulation matters;
- Claims for breach of confidentiality (due to wrongful disclosure of personal data) causing personal distress only. (See NHS (CNSGP) Regulations Section 5(1)(a) ).
- The following activities, unless they are being delivered under primary medical services contracts or are NHS ancillary health services under CNSGP:
1. Voluntary activities (including Good Samaritan/Good Neighbour acts) and overseas work;
2. Healthcare commissioned and provided by the Ministry of Defence; and GPs engaged by the Department for Work and Pensions (DWP) (except for completion of DWP forms required under a GMS contract which are in scope and therefore covered).
Please refer to the Scheme Scope document for detailed guidance on what falls within and without the scope of CNSGP.
Some primary care practitioners are required to purchase run off cover because they had non-occurrence based indemnity arrangements to cover clinical negligence claims arising from incidents before 1 April 2019. This only applies to primary care practitioners who had a claims-paid or claims-made indemnity arrangement or insurance policy at the time the incident occurred. It does not apply to MPS members or to MDDUS members who had an occurrence-based membership arrangement.
In addition to retaining the management of existing claims, and being involved in any run-off cover, MDOs or other indemnity providers continue to provide their members with advice and support on all non-NHS claims issues. For example, the following circumstances do not fall within CNSGP and so will be dealt with by your MDO or other provider:
- Non-NHS work;
- NHS Dentistry;
- Community pharmacy;
- NHS Optometry;
- Complaints (unless there is also a claim for compensation arising out of alleged clinical negligence);
- Inquests (unless there is also a claim for compensation arising out of alleged clinical negligence, in which case NHS Resolution will work closely with your MDO or other provider when dealing with the claim for compensation);
- Regulatory and disciplinary proceedings;
- Employment and contractual disputes;
- Non-clinical liabilities such as defamation.
You will need to maintain membership with an MDO or other indemnity provider in respect of activities and services not covered by CNSGP.
CNSGP provides cover on an occurrence based arrangement only, which means you are covered for any clinical negligence claim arising from an incident that occurred on or after 1 April 2019 – even where you have retired or ceased to work in general practice.
The new scheme mirrors arrangements in NHS trusts to bring significant benefits to general practice staff. NHS Resolution can already exercise discretion in relation to that scheme but rarely, if ever, does so. NHS Resolution will work hand in hand with those who find themselves the subject of a claim and only settle cases where compensation is due, while defending the rest. CNSGP is a comprehensive scheme available to all GPs and others working in general practice whether in GMS, PMS, APMS and other settings and GPs and general practice staff should be confident they are fully covered just as clinicians in secondary care are.
General practice staff who, for any period of time before 1 April 2019, held claims-paid or claims-made indemnity arrangements or insurance policies will need to purchase run-off or extended reporting period cover separately themselves to ensure that they are covered for incidents arising during the period they held such cover, unless the terms of their cover specify any defined circumstances where this would not be required. If you are unsure of your current indemnity arrangements then you should contact your existing indemnity provider.
Any clinical negligence liabilities arising from an act or omission occurring on or after 1 April 2019 are covered automatically by CNSGP. Therefore, you do not need separate cover for these liabilities. You can contact your MDO or indemnity provider to discuss any appropriate rebate of fees already paid.
If you receive a claim that relates to NHS treatment provided before 1 April 2019 and you are an existing or previous member of the MDDUS and/or the MPS, then you should report the matter to NHS Resolution via: elsgpnotifications@resolution.nhs.uk . If you are not/have not been a member of the MDDUS and/or the MPS, then please liaise with your MDO or other indemnity provider.
NHS Resolution is an arm’s length body of the Department of Health and Social Care. Our purpose is to provide expertise to the NHS on resolving concerns fairly, sharing learning for improvement and preserving resources for patient care.
If you have an ongoing case, you should have details of your dedicated case handler who can talk to you about any aspect of your case. NHS Resolution’s GP indemnity team has a wealth of expertise in managing clinical negligence claims across both primary and secondary care. NHS Resolution will instruct lawyers from its approved panel, all of whom are highly skilled and experienced in managing clinical negligence claims. If lawyers have been instructed to manage the claim on your behalf they will be your best first point of contact.
For any general queries, please contact NHS Resolution by:
1. Email – ELSGPnotifications@resolution.nhs.uk
– setting out the basis of your enquiry and we will either respond by email or telephone to discuss the issue further. Do not send any documents via email as they may contain patient sensitive data. Do not include any patient sensitive data in your email.
2. Telephone – call our Claims Helpline 0800 030 6798 at any time; 24 hours a day, 365 day a year to speak to a legal advisor about any clinical negligence claims covered by ELSGP, but not medico-legal matters, which will be handled by your MDO (or any other provider).
NHS Resolution’s aim is to help you to resolve any claim for compensation brought against you by a patient in relation to their clinical care under the NHS as fairly and as quickly as possible. Claims will be investigated thoroughly and compensation will be paid where our investigation confirms that this is due. We will seek your agreement to make admissions of liability, which mirrors our approach across all indemnity schemes operated by NHS Resolution (including the Clinical Negligence Scheme for General Practice and the Clinical Negligence Scheme for Trusts). Where appropriate we will defend the case on your behalf, calling upon the very best expertise to do so. In all cases, we will do all that we can to keep the matter out of formal court proceedings.
In the first instance you should speak with your MDO. It is important to do this as soon as you become aware of your involvement or potential involvement in an inquest, so they can provide you with as much support as possible. Late notification may limit the extent of assistance that can be provided by your MDO.
NHS Resolution will only become involved if a claim is intimated or likely. If you believe that being involved in an inquest is linked to an incident that could result in a potential claim under the Existing Liabilities Scheme for General Practice or whether a matter should be reported, please contact NHS Resolution by:
1. Email – nhsr.elsgpnotifications@nhs.net
– setting out the basis of your enquiry and we will either respond by email or telephone to discuss the issue further. Do not send any documents via email as they may contain patient sensitive data. Do not include any patient sensitive data in your email.
2. Telephone – call our Claims Helpline 0800 030 6798 at any time; 24 hours a day, 365 day a year to speak to a legal advisor about any clinical negligence claims covered by ELSGP and not medico-legal matters that will be handled by your MDO (or any other provider).
For guidance and background NHS Resolution has made three short films providing information on what to expect when called to an inquest. They can be viewed here.
No. The ELSGP (and the CNSGP) provides unlimited and comprehensive clinical negligence cover for the care, diagnosis and treatment of NHS patients. All compensation costs and legal costs will be met by NHS Resolution on your behalf, subject to compliance with scheme rules.
All providers of NHS primary medical services who were members of the MDDUS or MPS at the time that an incident occurred giving rise to an historic liability, and any practice staff working for the MDDUS or MPS member at the time of that incident, are covered under the ELSGP. This includes out of hours providers.
In addition to NHS primary medical services, any other NHS services provided by or for general practice are also covered under ELSGP (namely, NHS activities carried out by or for a provider whose principal activity is to provide NHS primary medical services). These ‘other’ NHS services are referred to as “ancillary health services”.
Those providers whose cover is with a medical defence organisation (MDO) other than the MDDUS or the MPS, are not currently covered by ELSGP and should continue to liaise with their MDO.
As above, ELSGP covers all providers of NHS primary medical services (and, in some instances, providers of NHS ancillary healthcare that was provided as part of, or for, general practice) who were members of the MDDUS or MPS at the time that an incident occurred giving rise to an historic liability, and any practice staff working for the MDDUS or MPS member at the time of that incident. This includes out of hours providers.
No other agreements with medical defence organisations or indemnity providers are in place. For now, non-MDDUS and non-MPS members should continue to liaise with their MDO or indemnity provider in the usual way.
The ELSGP is not a membership scheme. Individuals do not need to pay for ELSGP. If you have an ongoing claim that MDDUS is handling and which relates to an incident that occurred during your period of membership with MDDUS, then NHS Resolution, which is administering ELSGP on behalf of the Secretary of State for Health and Social Care from 6 April 2020 will, in the first instance, also be responsible for claims handling.
Some primary care practitioners are required to purchase run off cover because they had non-occurrence based indemnity arrangements to cover clinical negligence claims arising from incidents before 1 April 2019.
This only applies to primary care practitioners who had a claims-paid or claims-made indemnity arrangement or insurance policy at the time the incident occurred. It does not apply to MPS members or to MDDUS members who had an occurrence-based membership arrangement.
A claim is a formal request for compensation as a result of something that has gone wrong in relation to a patient’s healthcare. It should be made in writing and can come directly from the patient or a family member, or from their lawyer or representative.
The claims process is separate from a complaint or other investigation, although the same set of facts can give rise to both. Where a case includes multiple issues, such as an inquest and/or General Medical Council (GMC) proceedings, we will work closely with your medical defence organisation/indemnity provider to ensure that they are managed in a consistent manner.
Irrespective of whether a claim has been brought or is likely, it is extremely important that you are open and transparent with the patient and spend time with them to explain what has happened.
If their care was not as it should have been, you should apologise. An apology is not an admission of liability and should always be offered when something has gone wrong. Our guidance, “Saying Sorry”, is available here.
NHS Resolution’s aim is to help you to resolve any claim for compensation brought against you by a patient in relation to their clinical care under the NHS as fairly and as quickly as possible. Claims will be investigated thoroughly and compensation will be paid where our investigation confirms that this is due. Where that is not the case, we will defend the case on your behalf, calling upon the very best expertise to do so.
If you are an MDDUS member with an existing claim which was being handled by MDDUS prior to 6 April 2020, you do not need to re-notify this to NHS Resolution. The transfer of your claim has been handled directly between NHS Resolution and MDDUS.
If you receive a Letter of Notification or Letter of Claim (which are the two different pre-action documents which commence a claim) it is important that you contact NHS Resolution as early as possible as this will give us the best possible opportunity to protect your position and ensure that deadlines are met. You can find further details here.
It may also be appropriate to notify us of any incidents where a formal claim has not been commenced but is likely to be. Further details on what kind of incidents may be high risk for a claim are here. If you are not sure whether an incident should be reported you can contact NHS Resolution for advice.
Bear in mind NHS Resolution indemnity schemes do not cover any private (non-NHS work), nor activities outside of the scheme scope. If in doubt, you should discuss the particular circumstances or issue with your MDO or other indemnity provider or contact NHS Resolution.
If you have any concerns regarding whether a claim falls within ELSGP or whether a matter should be reported, please contact NHS Resolution by:
1. Email – ELSGPnotifications@resolution.nhs.uk – setting out the basis of your enquiry and we will either respond by email or telephone to discuss the issue further. Do not send any documents via email as they may contain patient sensitive data. Do not include any patient sensitive data in your email.
2. Telephone – call our Claims Helpline 0800 030 6798 at any time; 24 hours a day, 365 day a year to speak to a legal advisor about any clinical negligence claims covered by ELSGP and not medico-legal matters that will be handled by your MDO (or another provider).
It is essential when reporting a claim to NHS Resolution and providing documents that you do so securely to ensure that personal data (including but not restricted to that of a patient) is protected. When reporting a claim to NHS Resolution, complete the Claim Notification Form once it has been sent to you, and, where available, send us the following documents:
1. The section of the patient’s GP records which relates to the period of treatment which is the subject of the claim.
2. Letter of Notification or Letter of Claim or some other request for compensation from the patient or their solicitors;
3. Claim Form, Particulars of Claim – court documents commencing a clinical negligence claim;
4. All correspondence with the patient or their solicitors;
5. All correspondence relating to any complaint that may have been made by the patient;
6. Written comments, witness statements and reports you may have previously prepared, for example in preparation for a complaint response, inquest or regulatory hearing that relates to the relevant incident that is, or may be, the subject of a claim;
7. Any independent expert evidence that may have previously been obtained, for example in preparation for an inquest or regulatory hearing (if provided to you by your MDO);
8. Notes or associated documents from any inquest, including the details of the Coroner’s conclusion (if provided to you by your MDO); and
9. Any Serious Incident Investigation Report or any other report into a patient safety incident.
10. In addition, to the documents listed 2 – 9 above please provide details of any other legal or regulatory process relating to the same incident the subject of this notification to NHS Resolution, previously notified and managed by the MDDUS on your behalf.
The documents listed 2 – 9 above should not be included in a patient’s GP notes and should be kept separately. Where material, such as expert reports or witness statements, has been prepared in order to assist your personal defence in respect of another legal or regulatory process then you should discuss with your MDO or legal team before disclosing it to us.
These claims reporting guidelines will help beneficiaries of the Existing Liabilities Scheme for General Practice know when and how to report a claim.
NHS Resolution does not cover GMC inquiries and representation. You are advised to discuss circumstances with your MDO. If you believe that being reported to the GMC is linked to an incident that could result in a potential claim under the Existing Liabilities Scheme for General Practice or whether a matter should be reported, please contact NHS Resolution by:
1. Email – ELSGPnotifications@resolution.nhs.uk
– setting out the basis of your enquiry and we will either respond by email or telephone to discuss the issue further. Do not send any documents via email as they may contain patient sensitive data. Do not include any patient sensitive data in your email.
2. Telephone – call our Claims Helpline 0800 030 6798 at any time; 24 hours a day, 365 day a year to speak to a legal advisor about any clinical negligence claims covered by ELSGP and not medico-legal matters that will be handled by your MDO (or any other provider).
If you have any concerns regarding whether a claim falls within ELSGP or whether a matter should be reported, please contact NHS Resolution by:
1. Email – ELSGPnotifications@resolution.nhs.uk
– setting out the basis of your enquiry and we will either respond by email or telephone to discuss the issue further. Do not send any documents via email as they may contain patient sensitive data. Do not include any patient sensitive data in your email.
2. Telephone – call our Claims Helpline 0800 030 6798 at any time; 24 hours a day, 365 day a year to speak to a legal advisor about any clinical negligence claims covered by ELSGP and not medico-legal matters that will be handled by your MDO (or any other provider).
In summary, NHS resolution will be responsible for managing any claims for clinical negligence on your behalf. This will include:
- Carrying out investigations, including collation of documents, comments from those involved, preparing statements and obtaining evidence from independent experts;
- Providing advice on process, the legal framework and whether and acceptance of liability will be needed
- Managing the compensation, including an assessment of the value of the claim, whether any other parties should share responsibility and conducting negotiations and arranging for payments to be made
NHS Resolution will not be able to help with inquest and regulatory processes for which you should speak with your MDO.
Yes. For any ongoing cases, NHS Resolution will be in touch with you on how your cases will be managed and what you can expect from us.
For any new cases, shortly after notification, you will be provided with details on what to expect from the claims process and NHS Resolution.
NHS Resolution is a Special Health Authority with responsibility for providing indemnity in relation to clinical negligence claims against the NHS in England. Processing and storage of information is in accordance with our responsibilities under the General Data Protection Regulation and the Data Protection Act 2018. To learn more about how NHS Resolution will collect and use claims management data, please see our privacy policy here.
The Risk Pooling Schemes for Trusts (RPST) is the collective name for two separate schemes covering non-clinical risks, the Liabilities to Third Parties Scheme (LTPS) and the Property Expenses Scheme (PES).
The Liabilities to Third Parties Scheme (LTPS) typically covers employers’ and public liability claims from NHS staff, patients and members of the public. These range from straightforward slips and trips to serious workplace manual handling, bullying and stress claims. LTPS covers claims arising from breaches of the Human Rights Act, the Data Protection Act and the Defective Premises Act, as well as defamation, unlawful detention and professional negligence claims.
The Property Expenses Scheme (PES) covers “first party” losses for material damage to buildings and contents from a variety of causes, including fire, theft and water damage. PES also offers business interruption expense cover arising from property damage.
Coverage from both schemes within the RPST began on 1 April 1999. However, if an NHS organisation joined later than this date then they are covered from the day they joined.
The RPST schemes are funded by contributions from members and contributions are calculated on an annual basis using actuarial techniques, including the member’s previous claims experience.
NHS organisations may join either or both schemes with the RPST.
Arrangements are in place to indemnify healthcare professionals through one of the following state indemnity schemes:
a) The Clinical Negligence Scheme for Trusts (CNST), if they are engaged by an NHS trust to provide NHS services.
b) The Clinical Negligence Scheme for General Practice, if they are engaged by a GP practice to provide NHS services (i.e. a GP practice the main business of which is the provision of NHS primary medical services). This includes salaried GPs, locums, students and trainees, nurses, clinical pharmacists, agency workers and other practice staff.
During the outbreak, existing indemnity arrangements will continue to cover clinical negligence liabilities arising from the vast majority of NHS services, including staff working in a place that is not their ordinary place of work. To ensure there are no gaps in indemnity coverage, the Coronavirus Act 2020 provides additional powers to provide clinical negligence indemnity arising from NHS activities related to the Coronavirus outbreak, where there is no existing indemnity arrangement in place.
It provides cover for services directly related to coronavirus and for any backfill arrangements that may be needed, as a consequence of coronavirus, to sustain the delivery of NHS services.
We do not want indemnity to be a barrier or cause a delay to anyone assisting with the coronavirus response. We expect the vast majority of services will continue to be covered by existing indemnity arrangements. The indemnity provided under the Act provides a complementary indemnity on top of existing arrangements to ensure there are no gaps and provide reassurance to all staff who are asked to assist with the response.
All staff providing NHS services related to the coronavirus outbreak will be covered by this indemnity for clinical negligence where they are not already covered by an existing indemnity arrangement.
Where volunteers are asked by NHS trusts to help deliver NHS services, and a volunteer agreement is in place between the trust and the volunteer or volunteer organisation, then indemnity for clinical negligence will be provided under the Clinical Negligence Scheme for Trusts.
In most cases, returning healthcare professionals will be covered by one of the two existing state schemes: the Clinical Negligence Scheme for Trusts (CNST) if they return to work in an NHS trust; and the Clinical Negligence Scheme for General Practice (CNSGP) if they are engaged by a GP practice providing NHS GP services. However, in the rare instances where these or other indemnity arrangements do not apply, the indemnity provision under the Coronavirus Act will apply.
Yes, providing you are acting in the course of your employment. The key factors to consider are that healthcare professionals should at all times ensure they are competent to carry out any practice requested of them. If you are asked to work for an NHS Trust or GP practice, the existing state indemnity schemes will provide you with cover for clinical negligence arising from your activities. In the unlikely event that you are involved in the novel delivery of NHS services that fall outside the scope of these state schemes, you will be covered by the indemnity provision under the Coronavirus Act.
For details of what roles and working arrangements are in place for doctors please see details on the GMC website here, or the BMA here.
If the epidemic worsens it is likely that healthcare staff will have to work outside their normal field of practice. When deciding the safest and best course of action in the circumstances, healthcare staff should consider factors including what is within their knowledge and skills; the protection and needs of all patients they have a responsibility towards; and minimising the risk of transmission and protecting their own health.
Medical Defence Organisations (MDOs) advise that any doctor faced with clinical duties outside their clinical competence should explain their concerns clearly to someone with responsibility for providing the service to determine the safest way to proceed.
If they have done so and still feel uncomfortable, their MDO can advise them further. The GMC’s Good Medical Practice should be followed.
NMC have provided similar guidelines for Nurses and Midwives here.
The Devolved Administrations have taken an equivalent approach to England. While the existing state indemnity coverage is different in Scotland and Northern Ireland from that in England and Wales, the indemnity powers provided by the Coronavirus Act 2020 are comparable across the four nations. In all four nations staff providing NHS services related to the coronavirus outbreak will have indemnity under the Act, where they are not already covered by an existing indemnity arrangement.
Pharmacists and Pharmacy technicians working for general practice and NHS trusts are covered by state-backed indemnity schemes, and returning professionals engaged by NHS trusts or GP practices will also be covered by these schemes (irrespective of whether the services are provided in a hospital, a clinic, on GP premises, etc.):
- The Clinical Negligence Scheme for Trusts (CNST), see link here for details, if they are engaged by an NHS trust to provide the NHS services.
- The Clinical Negligence Scheme for General Practice (CNSGP) if they are engaged by a GP practice to provide NHS services (i.e. a GP practice, the main business of which is the provision of NHS primary medical services, see link here for details.
During the outbreak, existing indemnity arrangements will continue to cover clinical negligence liabilities arising from the vast majority of NHS services, including staff working in a place that is not their ordinary place of work. To ensure there are no gaps in indemnity coverage, the Coronavirus Act 2020 provides additional powers to provide clinical negligence indemnity arising from NHS activities related to the Coronavirus outbreak, where there is no existing indemnity arrangement in place. 5
It provides cover for services directly related to coronavirus and for any backfill arrangements that may be needed, as a consequence of coronavirus, to sustain the delivery of NHS services.
This includes any pharmacists that are requested, or volunteer, to assist with the Government’s NHS response to the Coronavirus pandemic.
Pharmacists and Pharmacy technicians are regulated health professionals and must ensure they have adequate indemnity insurance cover, either personally or through their employer. Community pharmacy contractors may also carry indemnity insurance for staff undertaking pharmaceutical services on behalf of the NHS. It is highly unlikely that professionals and staff in community pharmacy will be asked to do anything that is outside of standard NHS pharmaceutical services, so their normal indemnity insurance will cover them. As any new services are developed and introduced, we have committed to keeping the insurers updated so that they can flag any indemnity issues with us.
However, we do not want any indemnity concerns to be a barrier or delay to the response to the coronavirus outbreak. The powers taken in the Coronavirus Act 2020 allow the Secretary of State to provide indemnity for clinical negligence liabilities arising from NHS activities carried out for the purposes of dealing with, or in consequence of, the coronavirus outbreak, where there is no existing indemnity arrangement in place. Under these powers we have made provision for organisations or individuals undertaking NHS activities to respond to the coronavirus to be covered for clinical negligence in these circumstances. This includes those working in community pharmacy delivering pharmaceutical services for the NHS.
We recognise that returning doctors may also want to access medico-legal advice and support, and it is the Government’s intention to ensure this is not a barrier to their return. In Spring 2020, the Medical and Dental Defence Union of Scotland (MDDUS), the Medical Defence Union (MDU), and the Medical Protection Society (MPS) confirmed that they would provide medico-legal advice and support at no cost to their retired members who return to work on the Covid-19 response. For retired MPS and MDDUS members this was automatic. MDU asked retired members to complete a short form.
MDDUS and MPS are currently maintaining this position. MDU has written to its members to say that this no cost cover will be ending on the 30th September. Those MDU members with ongoing clinical commitments are encouraged to contact the MDU membership team to discuss their planned ongoing role and the membership options available to them.
More information for returning members is available via the respective websites of the three medical defence organisations. Please see the following:
We recognise that returning midwives may also want access to medico-legal advice and support, and it is the Government’s intention to ensure this is not a barrier to their return.
The Royal College of Midwives (RCM) has confirmed that it will extend all of the benefits of membership including Medical Malpractice Insurance (MMI) cover to any retired members who join the NMC’s emergency register for the duration of the Covid-19 outbreak.
RCM’s MMI will provide returning midwives with benefits and cover in addition to the vicarious primary liability provided by their NHE Employer, including insurance cover, legal advice and expenses and protection against claims for damages.
The terms and conditions of the RCM’s MMI are set out here.
The Royal College of Nursing has confirmed that if its student or retired members enter on to an emergency register at the NMC during the COVIS-10 outbreak, and if they need legal representation for employment or regulatory issues arising from their time on those registers, RCN will provide that representation even if their membership status remains that of student or retiree. Accordingly, there should be no barrier to them taking on new duties without any need to inform RCN, and they can be confident that the RCN will provide them with the same support as if they had a full membership. Further information can be found here.
The Pharmacists’ Defence Association (PDA) provides indemnity and legal defence costs insurance and individual representation where required to employed and self-employed pharmacists, as part of their standard wider membership offer which is entirely independent of any employer provided scheme. 7
The PDA have launched a new membership category specifically for retirees returning to practice because of the Covid-19 response at a preferential membership fee.
For further information please click here.
The Guild of Healthcare Pharmacists (GHP) recommend that, if you are a pharmacist returning to assist with the Covid-19 response, you are engaged to carry out your activities under a contractual arrangement with an NHS provider that states that indemnity will be provided for any liabilities arising from your work. The indemnity provided by the NHS provider (primary indemnity) should cover all aspects of your work for the provider. If, however, you need additional cover for anything not covered by the indemnity provided by your employer, your GHP membership with Unite the Union Contingent Medical Malpractice Cover (CMMC) will cover you for this. Unite’s CMMC comes into operation to protect you should your NHS employer’s primary indemnity not provide adequate cover, and provides cover for claims made against you (i.e. those not covered under your primary indemnity), your legal liability to pay compensation and any costs or expenses in respect of accidental personal injury.
For those returning pharmacists who are not GHP members, including registered community, academic and industrial pharmacists, GHP have negotiated a reduced rate for pharmacists to join GHP and provide you with CMMC for as long as you are employed to assist with the Covid-19 response. For further information please click here.
The Pharmacy Insurance Agency (PIA) is the main provider of professional indemnity and legal costs scheme for pharmacy technicians as part of their membership. The PIA has arranged a scheme specifically designed for those pharmacy technicians who are returning from retirement to re-register with the General Pharmaceutical Council (GPhC) to assist with the Covid-19 response. This new scheme is entirely independent of any employer-provided scheme and provides professional indemnity and legal defence costs insurance cover and is being offered at a preferential rate to returning pharmacy technicians.
For further information please click here.
Vets and veterinary nurses have been asked to assist with the Covid-19 response in a number of areas, primarily maintaining the food supply and supporting the livestock industry. However, vets and veterinary nurses generally have a broad clinical skill base and may, where they are not assisting elsewhere with the Covid-19 response, also be able to assist NHS Trusts in roles which are not reserved by law to licensed doctors or other registered professionals. 8
Vets and veterinary nurses are regulated by the RCVS and there are currently no proposals for emergency registration with other regulatory bodies such as the GMC or NMC.
NHS Trusts should ensure that any vets and veterinary nurses assisting with the Covid-19 response have clear job descriptions to satisfy themselves that they have the skills and competencies required. Where vets and veterinary nurses are working in NHS Trusts, indemnity cover will be provided under CNST for clinical negligence arising from the activities they carry out as they are being engaged to carry out NHS activities on behalf of the Trusts.
Where NHS staff are loaned/seconded to work in care homes or other social care settings to assist the delivery of social care, they should be covered by the indemnity arrangements of the care provider. All care providers are required to have insurance and suitable indemnity arrangements for the services they provide, and the care provider should provide assurance of these arrangements as part of the loan/secondment agreement.
NHS services delivered in a care home or other social care setting would be covered by the usual arrangements. For example, clinical negligence arising from NHS services provided by GPs or community trusts is covered by the Clinical Negligence Scheme for General Practice and the Clinical Negligence Scheme for Trusts, respectively. Scheme rules for CNSGP are given here and for CNST here.
Yes. CCG staff providing infection control training in care homes are covered for this activity by the CCG’s membership of the Liabilities to Third Parties Scheme run by NHS Resolution.
Yes, where you are appropriately trained and competent to undertake this activity, and you are not covered for this activity under your existing indemnity/insurance arrangements, you will be indemnified under the Clinical Negligence Scheme for Coronavirus (CNSC). The CNSC has been established by NHS Resolution to meet liabilities arising from the special healthcare arrangements being put in place in response to the coronavirus outbreak.
Antibody testing undertaken in NHS trusts will be covered under the Clinical Negligence Scheme for Trusts. Further information on the rollout of the antibody testing programme is set out in NHS England and Improvement’s letter on 25 May 2020.
Where possible, existing indemnity arrangements should cover dental nurses, including if you would usually rely on your employer’s indemnity cover rather than purchasing your own. However this cover may not extend to the urgent work that you may carry out for an NHS trust or another dental practice in a different location. If you are carrying out the urgent work for an NHS Trust in a place that is not your usual place of work, you will be covered by the Clinical Negligence Scheme for Trusts. If you are working in a high-street practice that is not your usual place of work and the work is being carried out for the owner of that high-street practice, you should in the first instance discuss with the new practice owner whether you will be covered by their indemnity policy. If this is not possible, the new Clinical Negligence Scheme for Coronavirus will cover you as a backstop.
If you are engaged by an NHS trust or a GP practice which provides NHS primary medical services, you will be indemnified under the Clinical Negligence Scheme for Trusts (CNST) or the Clinical Negligence Scheme for General Practice (CNSGP). NHS England and Improvement has also secured additional capacity through a series of contracts with independent sector hospital providers. Staff working under these contracts will be covered by CNSC.
The CNSC provides indemnity for clinical negligence liabilities arising from NHS activities carried out for the purposes of dealing with, or because of, the coronavirus outbreak. The scheme does not extend to the provision of private healthcare. If you are a healthcare worker practising in the independent sector and treating private patients, you will already have clinical negligence indemnity arrangement in place. If you intend to change your working practice you are advised to contact your indemnifier to ensure you continue to have appropriate indemnity.
Yes, providing you are acting in the course of your employment. The key factors to consider are that healthcare professionals, such as junior doctors, should at all times ensure they are competent to carry out any practice requested of them. During the outbreak, existing indemnity arrangements will continue to cover clinical negligence liabilities arising from the vast majority of NHS services, including staff working in a place that is not their ordinary place of work. In the unlikely event that existing indemnity arrangements do not apply, then the Coronavirus Act 2020 provides additional powers to provide clinical negligence indemnity arising from NHS activities related to the Coronavirus outbreak.
No. The indemnity powers in the Coronavirus Act 2020 will not be used to replace existing indemnity arrangements. The Act allows Government to provide indemnity to sit alongside existing indemnity arrangements to ensure there are no gaps in cover. This provision is designed to act as a ‘safety net’, for clinical negligence indemnity cover to be provided for NHS services related to the Coronavirus response, including any backfill arrangements that may be needed, to ensure the uninterrupted delivery of NHS services, where they are not already covered by existing indemnity arrangements.
Public health consultants returning to work for local authorities should check the cover position with the authority in question. Those returning to work for Public Health England will be covered for any clinical negligence arising from their work under state indemnity arrangements administered by NHS Resolution.
During the pandemic, clinicians including dentists continue to provide care in different ways to minimise the risk of infection. At times this has meant delaying care or providing a different standard of care. It is possible that claims will arise challenging these new practices, for example if a patient feels they were harmed by delays in seeing a dentist in person. As in usual times, dentists are expected to act in line with national protocols and are not liable for outcomes arising as a result of following those protocols. Any claims arising will be handled under the relevant indemnity arrangements as usual.
During the pandemic, dental staff have at times been asked to work at different practices. These staff will not always have their own clinical negligence indemnity arrangements, leaving the practice owner liable for their actions. If the practice owner’s existing indemnity arrangements do not cover staff they host from different practices, CNSC will provide cover for clinical negligence claims against the practice owner for actions of these staff.
We are responsible for managing clinical negligence claims brought against the NHS. Our role includes sharing learning to help improve patient safety and to preserve resources for patient care.
Clinical (or medical) negligence is when medical professionals or organisations, who owe a legal duty of care, do not meet the expected standard of care, causing injury to a patient or the patient’s condition becoming worse.
A three-part legal test needs to be carried out. You can find more information about this by watching the ‘Introduction to clinical negligence claims’ short video below.
NHS Trusts have to tell us about maternity incidents which meet a certain criteria. Under the EN Scheme, a team of clinicians and lawyers work together to investigate circumstances where babies have sustained specific brain injuries at birth to find out if the harm has been caused by clinical negligence. The team completes an early investigation into the care and provides compensation if their three-part legal test shows there has been clinical negligence. They also help NHS trusts take steps to learn from these incidents and work together to improve maternity and neonatal care (care in the first four weeks of a baby’s life). Please read the ‘How do you decide whether my baby is eligible for compensation?’ section below for more information about the legal test.
Babies who meet the criteria to be reported to us by NHS Trusts include full-term babies (at least 37 completed weeks of pregnancy) born following labour who have had a potential severe hypoxic brain injury confirmed on an MRI scan. This means that babies who are born by elective caesarean section, and babies who have sadly died within the first week of life (between birth and six days) will not be eligible for review under the EN Scheme.
A potential severe brain injury is diagnosed in the first seven days of a baby’s life. To diagnose this, one or more of the following must apply.
- The baby must have been diagnosed with moderate to severe hypoxic ischaemic encephalopathy (HIE). This is a brain injury caused by the baby’s brain not getting enough oxygen.
- The baby must have been therapeutically cooled (active cooling only). This is where their body temperature is lowered using a cooling mattress or cap, with the aim of reducing the impact of HIE.
- The baby must have had an altered state of consciousness, with seizures, weak muscle tone, abnormal reflexes or abnormal suck.
(The above is a simplified version of the Maternity and Newborn Safety Investigations (MNSI) criteria.)
These babies are reported to the MNSI programme.
The EN Scheme investigates a specific type of brain injury which meets our clinical MRI criteria.
We investigate cases involving therapeutically cooled babies where there is evidence of ongoing neurological injury (damage to the brain, spinal cord or nerves). This would usually mean that, to meet our investigation criteria, there will be a brain MRI scan showing evidence of intrapartum (during labour) hypoxic ischaemic encephalopathy (HIE). Intrapartum HIE is a type of brain injury that happens when the supply of oxygen to the brain is disrupted. We will assess cases reported to us to confirm if there is evidence of hypoxic injury on the MRI scan. Our clinical team will carry out an initial review, which will consider whether there are any initial concerns about the care you and your baby had and whether that care may have caused injury to your baby. If there are concerns that the care may have caused injury to your baby, we will carry out a full legal investigation. If your baby was born on or after 1 October 2023, we will ask for your permission to do this and ask you to sign a form giving us permission to access additional medical records.
The EN Scheme carries out an investigation to see if there was any clinical negligence.
The MNSI programme completes safety investigations which focus on systems and processes in healthcare, identifying the factors that could have led, or could lead, to harm for patients. It does not look at investigations from a legal perspective.
You can find more information about MNSI and their investigations on their maternity investigations page.
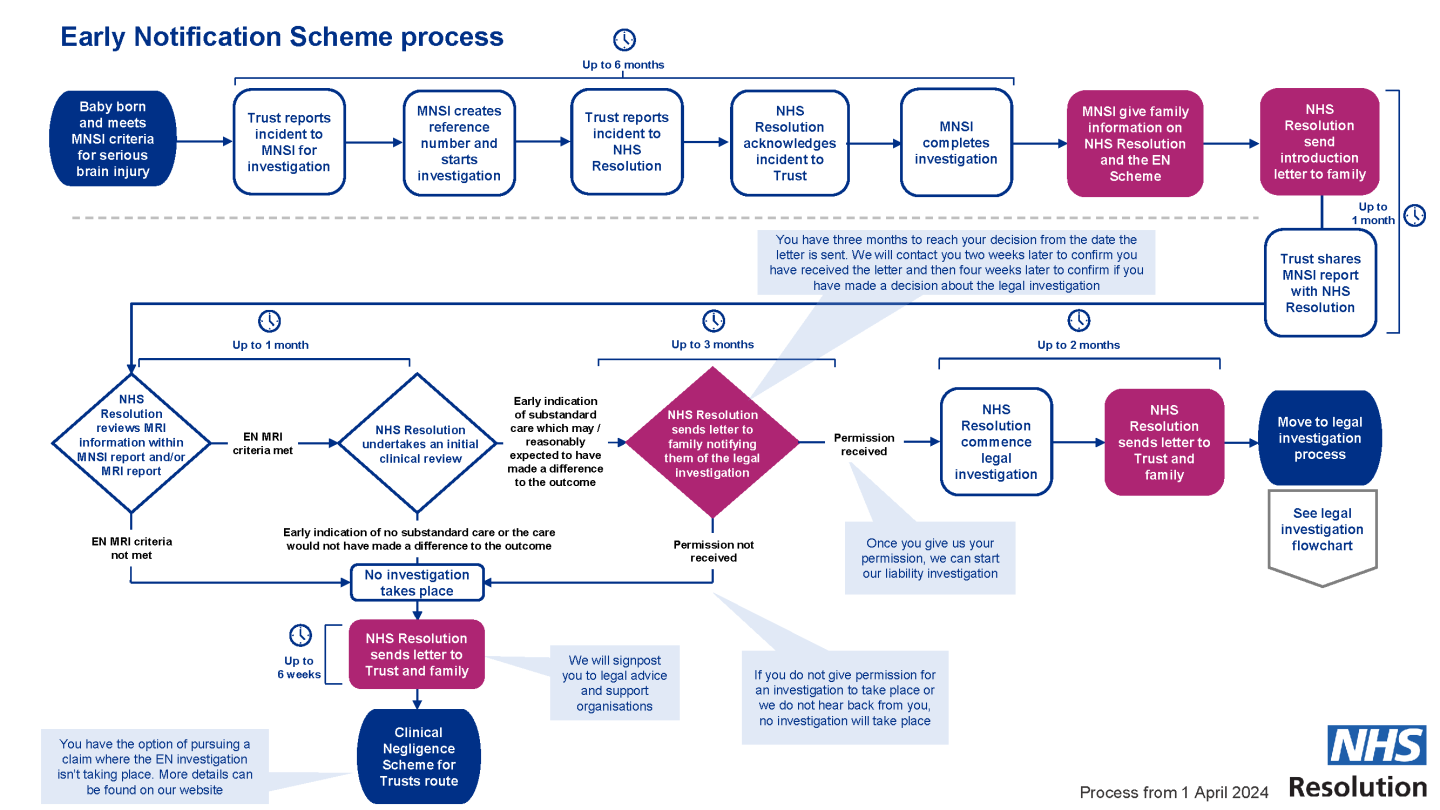
The flowchart below shows the steps of the investigation process for the EN Scheme investigation process.
If the harm was caused as a result of something a clinician did, or failed to do, while using their clinical judgement, clinical negligence law will determine whether you are entitled to compensation.
The flowchart below shows the steps of the legal investigation process.
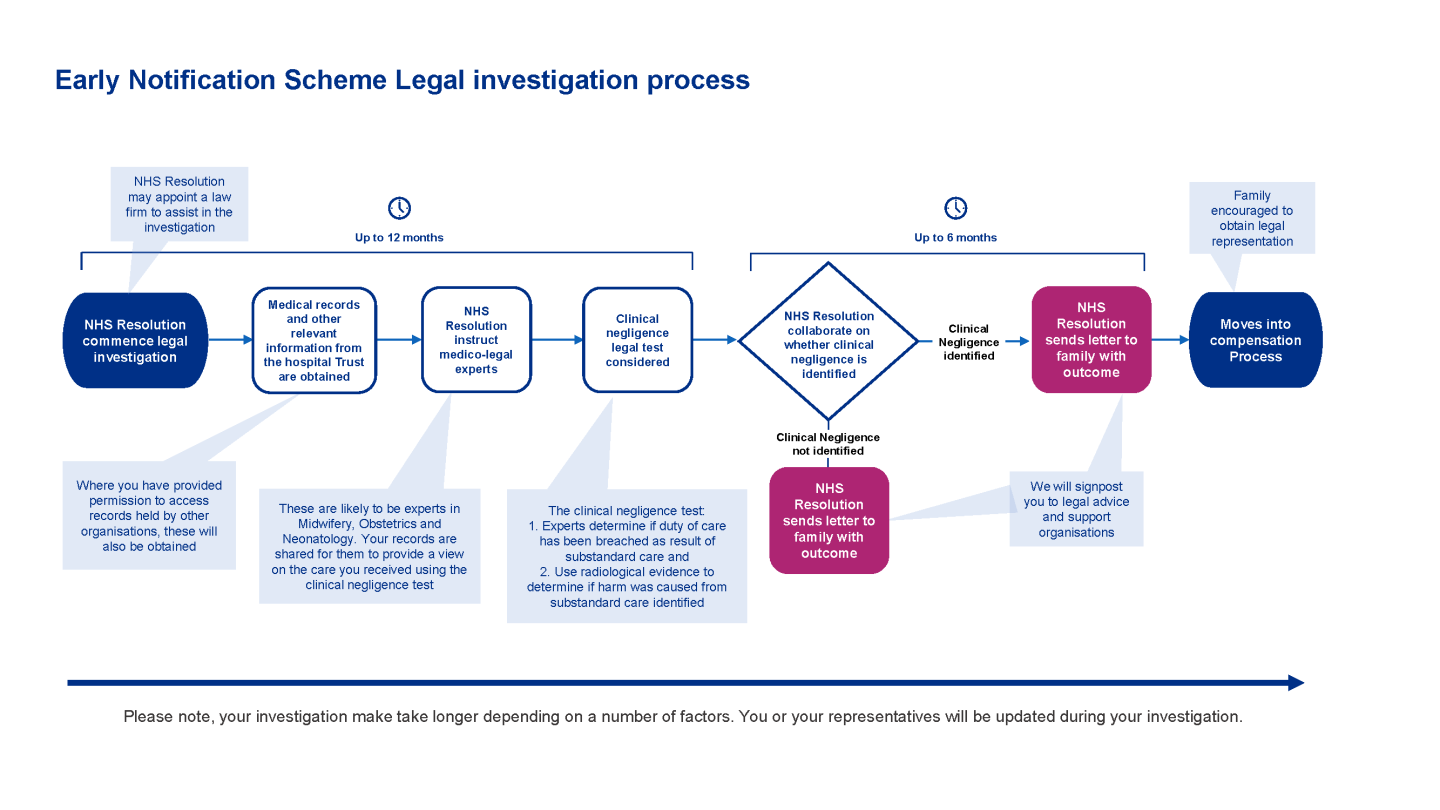
Summary of the legal investigation process
The hospital trust will report a baby’s birth which meets the scheme criteria to us. We will agree with you how often and in what way you would like us to contact you. If you instruct your own lawyers at any point, we will then communicate with them, rather than with you.
- Step 1: Once the hospital trust has received the report from the Maternity and Newborn Safety Investigations (MNSI) programme, they will share it with us. This is usually six months after your baby’s birth. We will check the details of your baby’s MRI scan (which takes up to one month), and if there is evidence your baby has an intrapartum hypoxic brain injury we will move to step 2.
- Step 2: We will carry out an initial review of your and your baby’s care and write to you with the outcome. If there are concerns that your care may have caused injury to your baby, we will carry out a full legal investigation. If your baby was born on or after 1 October 2023, we will ask for your permission to do this and ask you to sign a form giving us permission to access additional medical records (unless you have instructed lawyers by this point, in which case we will communicate with them). This step takes up to three months.
- Step 3: Once we have received your permission, we will contact you and explain the next steps.
- Step 4: Once we have received all the medical records from the various providers, we will share these with independent medical and legal experts who give their view on your care, using a legal test to assess whether you are entitled to compensation. The types of experts will vary, but often include a midwife, an obstetrician, a neonatologist and a neuroradiologist.
- Step 5: We will consider the experts’ opinions and may meet them to discuss your care. This is to decide whether the care caused or contributed to your baby’s injury, and whether you will receive compensation.
- Step 6: We will write to you or your lawyer with the outcome of the investigation. This detailed letter will explain whether your care was appropriate and whether or not there has been clinical negligence. You can then share the letter with any lawyer you instruct. This step takes about 18 months. (It may take longer than 18 months to receive this letter if we need to carry out further investigations.)
Documents produced when giving or receiving legal advice are protected under a principle called legal privilege. This means we will not be able to give you copies of the experts’ reports or other documents created during the investigation. Legal privilege also applies if you instruct your own lawyers.
You can get independent legal advice at any time. Or, you may want to wait until you have received our letter with the outcome of our investigation before considering whether to contact a specialist clinical negligence lawyer about making a claim.
You can find details of organisations that can support you by clicking on the support for patients, families or carers link.
The types of experts we instruct will vary, but often include a midwife, an obstetrician (a doctor specialising in pregnancy and labour), a neonatologist (a doctor specialising in looking after infants who are unwell after their birth) and a neuroradiologist (a doctor specialising in the interpretation of brain scans). In some cases a paediatric neurologist (a doctor specialising in diagnosing and managing neurological disorders in children) may also be instructed.
An expert’s duty is to the court. Their purpose is to provide a neutral opinion which is independent from us or the hospital trust. They advise on the standard of the care provided and whether, if that care had been different, your baby would have been less unwell following their birth. They will use the legal tests to help us and the trust establish whether there was clinical negligence.
The experts will consider the medical records and any other relevant documents, including incident investigation reports, local and national guidance and policies in place at the time of your care, and comments from staff who treated you and your baby. .
An expert’s duty is to the Court and their purpose is to provide neutral opinions which are independent from the Hospital Trust or NHS Resolution. They advise on the standard of the care provided and whether, if the care provided had been different, the baby would have been less unwell following birth.
The medical experts will need to review your medical records from your pregnancy, labour and birth. They will also need to see your child’s medical records (from birth onwards).
We have access to records held by the hospital trust where your child was born. The experts may also need to review records held by other healthcare providers, such as neonatal records from a different hospital trust if your child was transferred to a specialist unit after birth, their GP’s notes and other hospital notes, and those from other services (such as physiotherapy and occupational therapy). We will need your consent to access the records held by organisations other than the trust where you gave birth. If you have not already done so, please sign and return the consent form we sent you (the form of authority).
We will handle your records, and any information that arises from our investigation, sensitively and securely. When we need to share any information from the investigation, we will make that information anonymous before we share it. To find out more about how we will use this information, please see our privacy notice.
The following three-part legal test must be met for your child to be entitled to compensation as a result of clinical negligence. To see this information as a video or animation, please select here.
- Duty of care. Medical professionals have a duty of care (a legal obligation to ensure the safety and well-being of others). In most circumstances, a duty of care applies even if the medical professional is not your lead physician, and can apply to any clinical role, such as a doctor, nurse, midwife, nurse assistant, allied health professional or paramedic.
- Breach of duty. The duty of care must have been breached, meaning that the treatment received must have fallen below the standard considered to be proper by a reasonable and responsible group of clinicians (for example, midwives, nurses, doctors and so on) in the same situation.
- Causation. Once a breach of duty has been identified, it must be shown that it was likely that this caused harm or injury to you or your baby. There has to be a direct link between the care that fell below the required standard and any harm caused for the legal test to be met.
If breach of duty and causation are proven, the court will award financial compensation (otherwise known as damages).
The charity Action Against Medical Accidents provides useful explanations and self-help guides which provide further detailed information.
At the end of our investigation, we will send you a detailed letter with a summary of our findings and the reasons for them, including whether your baby is entitled to compensation.
We will not be able to give you copies of the experts’ reports or other documents created during the investigation. This is because documents produced when giving or receiving legal advice are protected under a principle called legal privilege. Legal privilege also applies if you instruct your own lawyers.
You can ask the hospital trust for copies of your medical records at any time, and you should also have received a copy of the safety investigation report from the MNSI.
If our investigation finds that the care fell below the expected standard, has caused an injury and there has been clinical negligence, your child will be entitled to compensation. We strongly advise you to get independent legal advice from a solicitor who specialises in these types of clinical negligence claims.
The next stage will be to carry out further investigations to decide how much compensation you will be paid. It can be difficult to assess the financial support your child will need, as they are still developing and the extent of their disability may not be known as their needs are changing.
It may take several years to agree a final settlement. In the meantime, the courts may award an interim payment to cover the costs of items or care your child needs immediately or in the near future. We will invite you and your representative to a meeting shortly after you have received the outcome letter. This meeting can be in person or online, depending on the circumstances. The aim of the meeting will be for us to better understand your child’s current condition and whether they have any needs which are currently not being met, and to get further information which can help us make interim payments.
We recommend that the lawyer accompanying you to this meeting is the lawyer acting for you and your baby, as they will be able to guide you through these discussions. If you have not yet appointed a solicitor, we can delay the meeting until you have found someone who you want to represent you.
There are strict legal rules about the time you have to make a claim for a child or parent, so we encourage you to get independent legal advice about this as soon as possible.
Helpful guides
- The patient safety charity, Action Against Medical Accidents (AvMA), have published guidance to help with calculating the time limit for making a claim. You can access this by scanning the AvMA QR code below or by typing the website address below into your web browser. https://www.avma.org.uk/wp-content/uploads/Legal-time-limits.pdf

- You can find more information on how to bring a claim by scanning the ‘Advice for claimants’ QR code below or by typing the website address below into your web browser. http://resolution.littlebirdwebservices.co.uk/services/claims-management/advice-for-claimants/

You can phone our EN team and its dedicated Family Liaison and Mediation Team on 0207 811 6263 (Monday to Friday 9am to 5pm) or email them at nhsr.enteam@nhs.net Where can I go for advice and support?
There are lots of organisations offering guidance and support for affected families. Please visit our website Support for patients, families or carers – NHS Resolution for more information.
Babies who meet the criteria to be reported to us by NHS Trusts include term babies born following labour (at least 37 completed weeks of gestation) who have had a potential severe hypoxic brain injury confirmed on an MRI scan. Babies who are born by elective caesarean section, and babies who have sadly died within the first week of life (0-6 days) will not be eligible for review under the EN scheme.
A potential severe brain injury is diagnosed in the first seven days of a baby’s life, and is when the baby:
- Was therapeutically cooled (active cooling only), or
- Has been diagnosed with moderate to severe encephalopathy, consisting of altered state of consciousness (lethargy, stupor or coma) and at least one of the following:
- hypotonia;
- abnormal reflexes including oculomotor or pupillary abnormalities;
- absent or weak suck;
- clinical seizures
(We have amended the wording on our family pages to give a simplified version of the above criteria).
These babies are reported to the Maternity and Newborn Safety Investigations (MNSI) programme.
The EN Scheme investigates a specific type of brain injury which meets NHS Resolution’s clinical MRI criteria.
We investigate cases involving therapeutically cooled babies where there is evidence of ongoing neurological injury. This would usually mean that to meet our criteria to be considered for investigation there will be a brain MRI scan showing evidence of intrapartum hypoxic ischaemic encephalopathy (HIE) (a type of brain injury that occurs when there is a disruption in supply of oxygen to the brain).
Cases reported in will be triaged to confirm if there is evidence of hypoxic injury on the MRI scan. Those cases confirmed as meeting the EN criteria will receive a preliminary review by NHS Resolution’s clinical team who consider whether there are any initial concerns about the care provided and whether that care may have caused injury to the baby. Where there are potential concerns about the care provided that may have caused injury to the baby, we will complete a full legal investigation. If the baby was born on or after 1 October 2023, NHS Resolution will ask the family’s permission to do this and ask for a signed form permitting us to access additional medical records.
Trusts are required to report all incidents that meet the Maternity and Newborn Safety Investigations (MNSI) programme criteria to MNSI and NHS Resolution. The criteria for an investigation by NHS Resolution’s Early Notification Scheme is narrowed to those cases reported to MNSI, where there is evidence of changes in relation to intrapartum hypoxic ischaemic encephalopathy (HIE).
The functions of MNSI and the EN scheme differ. There is some overlap between the organisations in that they both undertake investigations where a baby born at term has sustained severe brain damage following a delivery where there was labour. However, the EN criteria differs from the MNSI criteria as EN scheme will not investigate intrapartum stillbirths, maternal deaths or early neonatal deaths (within the first week of life (0-6 days).
It is important to note that whilst there is some overlap in the investigations undertaken by both organisations the purpose of MNSI and EN scheme investigations differ. MNSI investigations and reports are prepared with a view to making recommendations with the aim of improving healthcare systems and processes and reducing risk of harm to patients. NHS Resolution employs a litigation lens to the incident to assess the standard of medical care provided, which is different to the assessments made by MNSI investigators.
MNSI carry out their safety investigation and once completed NHS Resolution overlays an investigation to identify cases that satisfy the legal requirements for financial compensation. So, whilst the two organisations may review and investigate the facts of the same incident the remit and purposes of the two organisations are distinct.
Trusts are reminded that Safety Action 10 of the Maternity Incentive Scheme requires trusts to report 100% of qualifying cases to MNSI and to NHS Resolution’s EN scheme. Therefore, the reporting requirement and responsibility remains with trusts.
* Due to extreme circumstances caused by the Covid-19 pandemic crisis data sharing arrangements were put in place between MNSI and NHS Resolution to ease extreme work pressures faced by Trusts during this period. With the end to the pandemic the data-sharing arrangements put into place have expired and we have now reverted to pre-Covid reporting requirements.
The EN scheme has strict entry criteria, so where MNSI may review and report on an incident due to family or Trust concerns, the EN scheme will not investigate cases where there is a normal MRI (because they do not meet the minimum entry requirements for the EN scheme).
In such circumstances, Trusts may wish to signpost families to the ‘support organisations’ section of the EN scheme family and carers webpage where there are details of organisations that may be able to provide them with legal advice and specialist support. You can also signpost them to our ‘Advice for claimants’ webpage where the family can find more information about how to make a claim where an EN investigation isn’t taking place.
In circumstances where the EN scheme criteria has been met but the family decline an MNSI investigation, they can still request an EN review independently of MNSI.
In these circumstances the Trust should:
- notify the EN team by reporting the matter via the Reporting Claims Wizard
- mark the EN report form to reflect the families’ wish for an EN review where they have declined an MNSI investigation
- provide the relevant documents to enable NHS Resolution to conduct a preliminary triage (MRI report and child’s condition at discharge in the first instance). The EN team will be in touch to request other medical records or documents if needed.
Please note this is the only exception to the rule that all EN cases must be reported to the EN scheme with the relevant MNSI reference.
Trusts are reminded that the EN preliminary criteria stipulates that as a minimum the baby must survive to day seven and beyond. Unfortunately, babies that die within the first week (zero to six days) fall outside of the EN scheme.
If an incident initially meets the EN criteria and is reported to NHS Resolution and the child subsequently dies (some time beyond day seven) this does not preclude the case from proceeding under the EN scheme.
Trusts are reminded that in circumstances where a child subsequently dies or there are other significant clinical developments after a case is reported to the EN team we expect that this information is reported to the EN team case manager as soon as possible and without delay. It is of paramount importance that we have all of the relevant up to date information relating to a case provided to us and recorded on the file. This will minimise the risk of causing unnecessary distress or upset to the family when we are in contact with them.
Initially where the MNSI criteria are met but they subsequently decline to investigate the matter because there is a normal MRI the incident is not reportable to the EN scheme. In these circumstances, please follow your Trust’s framework for responding to patient safety incidents for the purpose of learning and improving patient safety.
Unfortunately, we are unable to amend the Reporting Wizard as this is a portal used by members to report different types of claims to NHS Resolution not just the EN scheme.
To avoid rejection of the case when reporting EN matters please ensure that:
- the MNSI reference is set out in the ‘Any other comments’ box on the Reporting Wizard AND
- the MNSI reference number is also set out on the EN Report Form.
We have listed the following steps to outline when to notify ENS:
Step one
Please report qualifying incidents to MNSI as per the MNSI criteria.
Step two
Case is deemed eligible and/or is accepted for investigation by MNSI.
Babies who meet the criteria to be reported to us by NHS Trusts include term babies born following labour (at least 37 completed weeks of gestation) who have had a potential severe hypoxic brain injury confirmed on an MRI scan. Babies who are born by elective caesarean section, and babies who have sadly died within the first week of life (0-6 days) will not be eligible for review under the EN scheme.
A potential severe brain injury is diagnosed in the first seven days of a baby’s life, and is when the baby:
- Was therapeutically cooled (active cooling only), or
- Has been diagnosed with moderate to severe encephalopathy, consisting of altered state of consciousness (lethargy, stupor or coma) and at least one of the following:
- hypotonia;
- abnormal reflexes including oculomotor or pupillary abnormalities;
- absent or weak suck;
- clinical seizures
(We have amended the wording on our family pages to give a simplified version of the above criteria).
These babies are reported to the Maternity and Newborn Safety Investigations (MNSI) programme.
The EN MVAG was established to provide external stakeholders, in particular families and their representatives, with a forum through which they can advise and support future service developments within the EN scheme.
MVAG currently includes representatives from Campaign from:
- AvMA (Action against Medical Accidents)
- Baby Lifeline
- Peeps HIE Charity
- Campaign for Safer Births
- Maternity Newborn Safety Investigations programme
- Russell-Cooke legal firm
- Capsticks Solicitors LLP
- NHS Resolution
It is our ambition that the group will become a forum for the NHS Resolution EN team and key stakeholders to:
- Work creatively to co-produce solutions together such as EN patient facing products or materials
- Use patient experience data and insight to inform future development of the EN Scheme
- Evaluate and provide opportunities for continuous quality improvement through shared learning from incidents.
For Trusts wishing to direct staff members involved in an incident towards further support and advice there is also some guidance and information as well as a list of organisations that may be able to provide them with further assistance within Appendix 1 of the Early Notification Second Report.
In such circumstances the Trust may wish to signpost families to a charity called Peeps H.I.E. which provides support and advice to families affected by babies born with hypoxic ischaemic encephalopathy (HIE).
You may also wish to direct families to the EN family facing page as we list several other organisations that may be able to provide them with specialist legal advice and support.
If the incident does not meet the EN entry criteria it will fall outside of the EN scheme. Trusts can direct families to the EN family facing page where we provide a list of support organisations that may be able to provide them with specialist legal advice and support.
Trusts can signpost families directly to the charity Action for Medical Accidents (AvMA).
The EN scheme recognises that any time an adverse outcome occurs it affects the patient and family but can also be emotionally difficult and stressful for the staff involved. NHS Resolution is unable to provide support directly to individual staff members, therefore staff support should be provided at a local level in the first instance. Our ‘Being Fair’ report promotes a just and learning culture within organisations and illustrates how staff should expect their organisation to support them. Improved support for affected staff members was also one of the recommendations contained within the EN scheme’s first and second reports and within Appendix 1 of the EN Second Report we list some further resources that may assist staff members involved in an adverse incident at work.
In the meantime, the EN scheme aims to make the EN investigation and process as stress free as possible for staff members. EN scheme clinical and legal team members are available to discuss staff member queries relating to the EN scheme and investigation process via email or telephone (nhsr.enteam@nhs.net or 020 7811 6263).
Trusts are reminded that Safety Action Ten of the Maternity Incentive Scheme mandates all qualifying incidents to be reported to MNSI and the Early Notification Scheme.
Please check the EN entry criteria for more information on qualifying incidents.
Please note that the EN scheme does not investigate maternity incidents where there was an elective caesarean section.
The EN requirement regarding labour aligns with the MNSI’s criteria for labour which is defined as follows:
- Any labour diagnosed by a health professional, including the latent phase (start) of labour at less than 4cm cervical dilatation.
- When the mother called the maternity unit to report any concerns of being in labour, for example (but not limited to) abdominal pains, contractions, or suspected ruptured membranes (waters breaking).
- Induction of labour (when labour is started artificially).
- When the baby was thought to be alive following suspected or confirmed pre-labour rupture of membranes.
The EN investigation may involve the instruction of Panel solicitors (specialist healthcare lawyers who are instructed to act on behalf of NHS Resolution and their Member Trusts). These lawyers will go on to instruct medical experts who provide independent opinions on the care provided.
The types of experts instructed will vary but often include a midwife, an obstetrician (doctor specialising in pregnancy and labour), a neonatologist (doctor specialising in looking after infants who are unwell after their birth) and a neuroradiologist (doctor specialising in the interpretation of brain scans). In addition, some cases will also have a paediatric neurologist instructed (doctor specialising in diagnosing and managing neurological disorders in children).
An expert’s duty is to the Court and their purpose is to provide neutral opinions which are independent from the Hospital Trust or NHS Resolution. They advise on the standard of the care provided and whether, if the care provided had been different, the infant would have been less unwell following birth.
An EN expert summit is a forum where multiple EN cases can be considered at a single point in time. This allows for discussions between medico-legal experts, a senior barrister, the instructed panel solicitor and NHS Resolution as well as representatives from the member trust. The discussions remain subject to legal privilege as they are primarily for the purposes of obtaining information and advice in the context of reasonably contemplated litigation. Key information is captured, tested and considered to allow counsel and solicitors to set out a road map towards providing an open and considered letter of explanation to the family. This includes early admissions of liability and apologies where appropriate. Where further investigation is identified, then further actions will be agreed between the parties at the Expert Summit.
Trust representatives will normally be invited to attend an expert summit. It is often very useful to have clinicians in attendance at expert summits because they frequently provide many helpful factual insights in discussions between experts and the senior barrister which may otherwise not be known.
Panel firms and NHS Resolution will coordinate summits and arrange the date and time for these. Some months prior to the summit the EN case manager and panel lawyer will take a view as to whether trust clinicians should be invited to attend. Panel will liaise with the Trust legal team to invite either the treating clinicians or someone more senior who may be able to provide information or necessary approvals. If clinician attendance is required, we will contact the Trust legal team to arrange this.
Documents produced when giving or receiving legal advice are protected under a principle called “legal privilege.” This means we will not be able to give the family copies of the expert reports or other documentation created during the investigation. Legal privilege also applies if the family instruct their own lawyers.
If the EN investigation identifies substandard care that has caused an injury, and negligence is determined, the injured child will be entitled to compensation, and we will strongly advise the family to obtain independent legal advice from a solicitor who specialises in these type of clinical negligence claims.
The next stage will be to carry out further investigations to establish the amount of compensation to be paid. It can be difficult to assess the level of financial support a child will need as they are still developing, and the extent of their disability may be unknown, as their needs are changing. It may take several years before a final settlement can be agreed but in the meantime the courts may award what is known as an ‘interim payment’ to cover the costs of items which are required immediately or in the near future. The family and their representative will be invited to attend a meeting shortly after they have received the outcome letter (this can be in person or virtual/remote depending on circumstances). The aim of this meeting will be for us to better understand your child’s current condition, whether there are any needs which are currently unmet, and to gain further information which can assist us in making early interim compensation payments.






