Insight report resource

Key messages and actions
- Practitioner Performance Advice (Advice) commissioned research into the lived experience of ethnic minority1 and international medical graduate (IMG) practitioners with our service and their employers to produce practical suggestions to provide a fair, consistent service to all where there are performance concerns.
- The findings provided a mixed picture in terms of whether practitioners felt they had been treated fairly by Advice and their employer; most participants described feeling discriminated against and long-term impacts included trauma, stress and anxiety.
- Advice acknowledges the experiences and the significance of the impact on individuals. We have developed actions rooted in these experiences to improve our service for all practitioners.
- Furthermore, we are sharing learning and collaborating with employers and national bodies to support positive change in the management and resolution of concerns throughout the system.
- We encourage employers to consider the findings of this research in light of the NHS equality, diversity and inclusion (EDI) improvement plan, which sets out why EDI is a key foundation for creating a caring, efficient, productive and safe NHS.
- Download the full report
- Download Case study 1: Health concern, positive experience
- Download case study 2: Behaviour concern, negative experience
Why did we commission this research?
NHS Resolution is committed to supporting the fair management and resolution of concerns including through our range of services, the ‘Just and learning culture charter’ included in our publication Being fair 2 and through collaboration with NHS England on the Medical Workforce Race Quality Standard (MWRES).
We know from our own and other research that ethnic minority and IMG practitioners are more likely to enter disciplinary processes2, have higher rates of cases with our service3 and “black and minority ethnic backgrounds have a poorer experience of medicine than their white colleagues”4. Furthermore a recently published survey of Black and ethnic minority NHS staff’s lived experiences of raising allegations of racism within their organisations found that the most common reason for not raising a concern about race discrimination was not believing anything would change (75.7%) and of those who did raise concerns, only 5.4% said they were taken seriously and that their problem was dealt with satisfactorily5 .
Practitioner Performance Advice commissioned this research to gather richer insight and further our understanding of the lived experience of ethnic minority and IMG practitioners with our service as well as their wider experiences of the management of concerns about their practice. The research is in line with our strategic commitments to share data and insights as a catalyst for improvement and to deliver fair resolution in our casework.
Ultimately, having a better understanding of the experience of practitioners will allow us and healthcare organisations to continue to improve how cases are managed and help us interact with practitioners in a more compassionate way by ensuring they feel heard, supported and understood.
EDI is everyone’s business – our leaders set the tone and culture, but we all have a role to play. Progressing the EDI agenda requires not only a change in systems and processes, but also cultures and behaviours.
NHS equality, diversity, and inclusion improvement plan
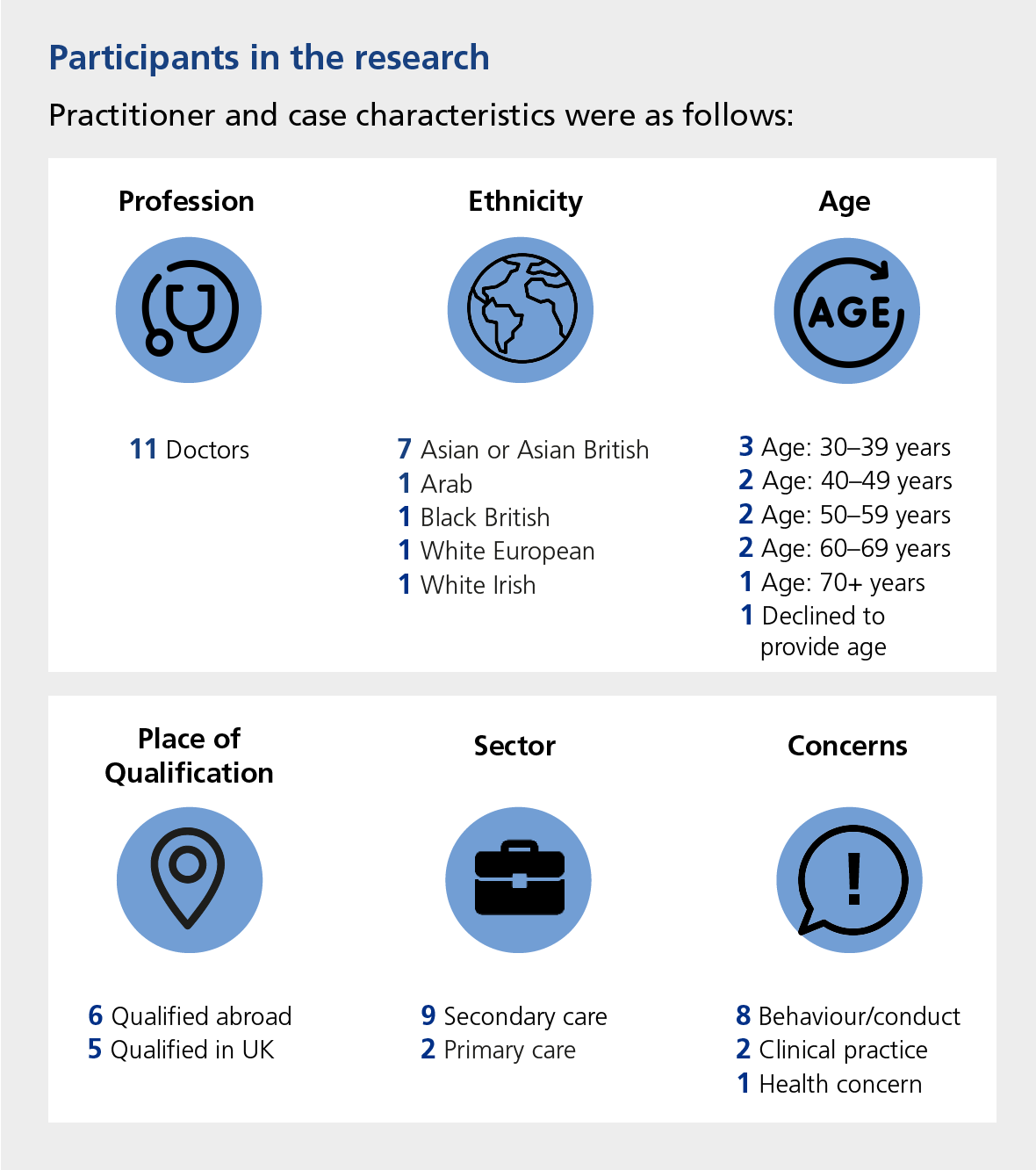
What did the research involve?
In order to gather perceptions and experiences, in-depth interviews were conducted with 11 practitioners from ethnic minority backgrounds and/or those who are IMGs who were the subject of cases with the Advice service. The interviews were conducted independently by Opinion Research Services (ORS). The experiences shared and included in the report primarily reflect the handling of the case by the employer6 and the Advice service.
Findings
The below infographic highlights key themes and quotes from the report and a range of experiences. Much more detail is included within the report itself.
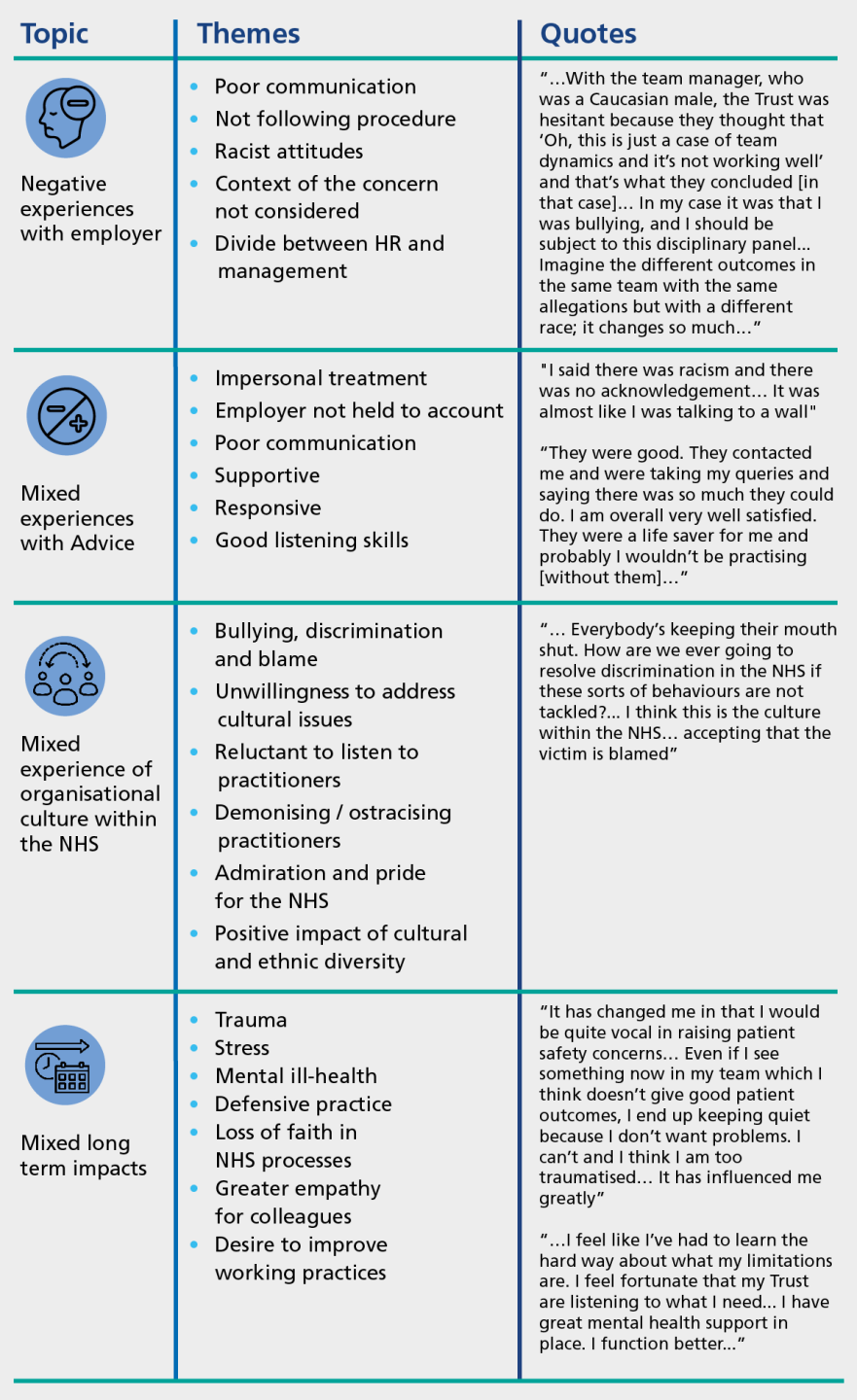
Most participants had very little knowledge about how their performance concerns would be handled and few understood the role of Advice in the process.
Most participants felt discriminated against based on their ethnicity and/or where they qualified. They felt this was reflected in the way their cases were handled by both their employer and Advice, and the higher rates of concerns raised against practitioners from ethnic minority backgrounds.
Most participants did not feel they had been treated fairly by their employers. Reasons for this included that employers had not followed proper procedures when handling concerns, and the perceived divide between clinicians and HR/management. There was a definite sense that those who deal with concerns and allegations internally are somewhat remote from the day-to-day clinical environment, and thus lack the understanding and empathy to look at the situation holistically.
Participants expressed mixed views on whether Advice had treated them fairly. Some felt they had been treated fairly because Advice listened to them and took all relevant information into account. Conversely, others did not feel treated fairly because Advice did not verify information employers gave them regarding concerns and did not consider the full range of information in relation to concerns.
Most participants described a culture of bullying, discrimination and blame within the NHS, and an unwillingness to address it. They also felt that the NHS is reluctant to listen to practitioners’ concerns, often demonising and ostracising them. Examples were provided about concerns about patient safety not being listened to, experiences of racial discrimination being disregarded and extenuating circumstances not being taken into account. However, some practitioners expressed pride and admiration for the NHS.
How Advice have responded to the research
There was a strong sense from participants that it is now time to put in place actions to address the disproportionate numbers of ethnic minority and IMG practitioners subject to disciplinary procedures. Advice fully acknowledges the experiences shared by practitioners and the significance and toll of the impact on individuals and their families.
Our initial response has been to develop actions rooted in these experiences to improve our service for all practitioners. The work we are doing is continuing to evolve and is outlined below:
1. Advice’s initial action plan
Our initial action plan outlines a range of internal actions for the Advice service to take forward to improve the fairness and transparency of the service for all practitioners.
2. Advice EDI Working Group
The actions from the initial action plan have been drawn into a broader programme of EDI activities which are being overseen by an internal working group chaired by Vicky Voller, Director of Advice and Appeals.
Our EDI group has a clear vision for the change we want to achieve:
Practitioners working in the NHS have an equitable and fair experience of the management of concerns about their practice which is not affected by their diversity.
3. Working collaboratively with other organisations
We have held workshops and briefings with practitioner groups, employers, defence organisations and national bodies, including regulators, to share this research widely to maximise learning and identify areas for collaboration. Furthermore, given our unique position in the healthcare landscape, we are taking a convening role to advance EDI work through initiatives focused on developing processes, early resolution, guidance and education. The Advice service is not a regulator, decision making body, trade union or medical defence organisation but we are sharing learning with these organisations and working together to improve fairness for all.
What will employers see Advice doing differently?
As an employer who contacts us for advice or uses our services, you will see us doing the below:
✔ Contact with practitioners: We will ask you to notify practitioners of Advice involvement promptly unless there is a compelling reason not to do so. We will also encourage employers to give regular updates to practitioners on the progress of the case.
✔ Checklist: We are in the process of developing of a checklist to support employers to take a proportionate and fair approach to the preliminary analysis of concerns, as part of our commitments to MWRES; The First Five.
✔ Discriminatory behaviour: If a practitioner shares concerns with us that they are being discriminated against, we will agree with the practitioner the best way to take forward so that their concerns are heard by their employer. Additionally, where we perceive there are unfair or discriminatory behaviours or actions, we will escalate this through the appropriate channels.
✔ Over-representation of ethnic minority and IMG practitioners: Reflecting data on practitioner demographics back to employers as part of discussions about ‘organisational activity reports’. This will allow healthcare organisations to reflect on themes and trends over time and consider any improvement action in relation to managing performance concerns and remediation. If you are reading this as a healthcare employer and are interested, please contact us at: nhsr.casesupport@nhs.net
What will change for practitioners?
If you are a practitioner where Advice is involved in your case, you will see the following:
✔ Responding to discrimination: Where practitioners report that employers have displayed racism or any other form of discrimination, Advice will identify the appropriate channels to share and escalate the matter.
✔ Clearer communication from Advice: We have produced a resource to clarify our role and what Advice can do for both practitioners and employers. This outlines that we can provide general information to help a practitioner better understand relevant aspects of the performance management process. Our team will also continue to signpost practitioners to appropriate sources of tailored support. We are working on communication improvements so that initial and ongoing contact with practitioners is made in a sensitive and appropriate way.
✔ Better communication from your employer: We will encourage employers to notify practitioners of the involvement of Advice and provide you with regular updates about your case.
What should employers do next?
We invite employers to read the report and case studies and to ask yourself the following questions:
- Are any of the experiences or themes present in cases I am managing?
- How can I ensure management of concerns is fair for all at my organisation?
- What can I do to ensure my organisation has a culture free from discrimination and bullying?
- Do we contact Advice early enough? There is no threshold for contact with the Advice service and earlier involvement of Advice may lead to earlier resolution.
- Could my organisation benefit from the revised Just and learning culture charter at the end of Being fair 2 or education courses?
- If you are an employer and interested in discussing your organisational activity report to reflect on themes and trends in your cases over time, please contact us at: nhsr.casesupport@nhs.net
- Who should I share and discuss this Insight with?
Furthermore, we encourage employers to consider the findings in light of the NHS equality, diversity, and inclusion improvement plan. In particular, our approach may support employers with ‘High impact action 1’, demonstrating how organisational data and lived experience have been used to improve culture and reviewing relevant data to establish EDI areas of concern and prioritise actions. The questions used in the research interviews are at the end of the report and could provide a framework for understanding lived experience in local organisations.
Thank you
ORS and Practitioner Performance Advice would like to thank the participating practitioners for sharing their experiences so openly and candidly. ORS and Practitioner Performance Advice recognise that sharing their experiences may have been difficult for practitioners and are grateful that they gave their time and effort to this work.
Our Insights publications share analysis and research which draw on our in-depth experience providing expert, impartial advice and interventions to healthcare organisations. By sharing these Insights, we aim to support the healthcare system to better understand, manage and resolve concerns about doctors, dentists or pharmacists. You can find all past reports on our Insights home page.
If you are interested in hearing more about our research and insights programme, please get in touch with us at: nhsr.adviceresearchandevaluation@nhs.net.
If you’d like to learn more about our work and the services we offer, please visit our dedicated Practitioner Performance Advice webpages. Our Education service offers training courses to provide healthcare organisations with the knowledge and skills to identify and manage performance concerns locally.
Footnotes:
1. A note on terminology: As an arms-length body of the Department of Health, we have followed government guidance, Writing about ethnicity. When citing other sources, we have reproduced the terminology used in the source.
2. Fair to refer?, GMC, 2019
3. Demographics, professions and concerns: What are the patterns in Practitioner Performance Advice cases?, NHS Resolution, 2023
4. Medical Workforce Race Equality Standard (MWRES); A commitment to collaborate The First Five , NHS England, 2023
5. Too hot to handle? Why concerns about racism are not heard or acted on, brap and Roger Kline, 2024
6. Primary care practitioners may be part of a contractual rather than an employment relationship. For ease of reference, we have used ‘employer’ throughout this Insight.






