Demographics, professions and concerns: Patterns in Practitioner Performance Advice cases with a focus on IMGs
NHS Resolution’s Practitioner Performance Advice service (Advice) is committed to providing a service to frontline healthcare organisations and practitioners that feels fair and equitable while concerns about individuals’ practice are managed and resolved, with the aim of supporting the NHS clinical workforce to deliver safe and effective patient care. To support this ambition, we are pleased to publish our annual analysis of the patterns of concerns reported to us by healthcare organisations and practitioners, as well as the demographics of the practitioners, in our casework over a five-year period between April 2019 and March 2024.
This year we are providing additional analysis focusing on our casework involving international medical graduates (IMGs) to inform and progress actions across the healthcare sector to improve fairness in how concerns are managed and resolved. We are also highlighting our Organisational Activity Reporting (OAR) service as a tool for secondary care employers who can explore their own data with the support of the Advice service to aid the fair and effective management of cases locally.
Key headlines
- Behaviour/misconduct features in 73% of the cases, similar to our previous periods of analysis.
- Ethnic minority, IMGs, older and male practitioners continue to be overrepresented in concerns reported to us by employers and contracting bodies.
- IMGs appear overrepresented in GP training grades and there are higher proportions of cases for IMGs who have been in a role for under one year.
- NHS Resolution is committed to supporting the fair management and resolution of concerns by working with healthcare organisations through our range of services, sharing learning from our lived experience research and engaging with healthcare partners on Equality, Diversity and Inclusion (EDI) initiatives.
Key actions for managers of performance concerns
- We ask senior leaders of healthcare organisations to consider using and signposting practitioners to NHS Resolution’s Advice service to provide impartial advice. This enables a fair and effective application of the healthcare organisation’s own local performance management, associated procedures and good practice in relation to local case management and investigation.
- If you are responsible for the management/oversight of concerns about individual clinicians at a secondary care trust, you can request your own OAR to support the fair and effective resolution of individual team and performance concerns. The OAR helps to identify patterns and issues in casework, providing insights to strengthen local performance management and improve frontline understanding of the causes of concerns. You can discuss your report with your organisation’s Link Adviser who will provide an independent view on your report, making use of their experience and expertise in performance management.
Pattern of concerns
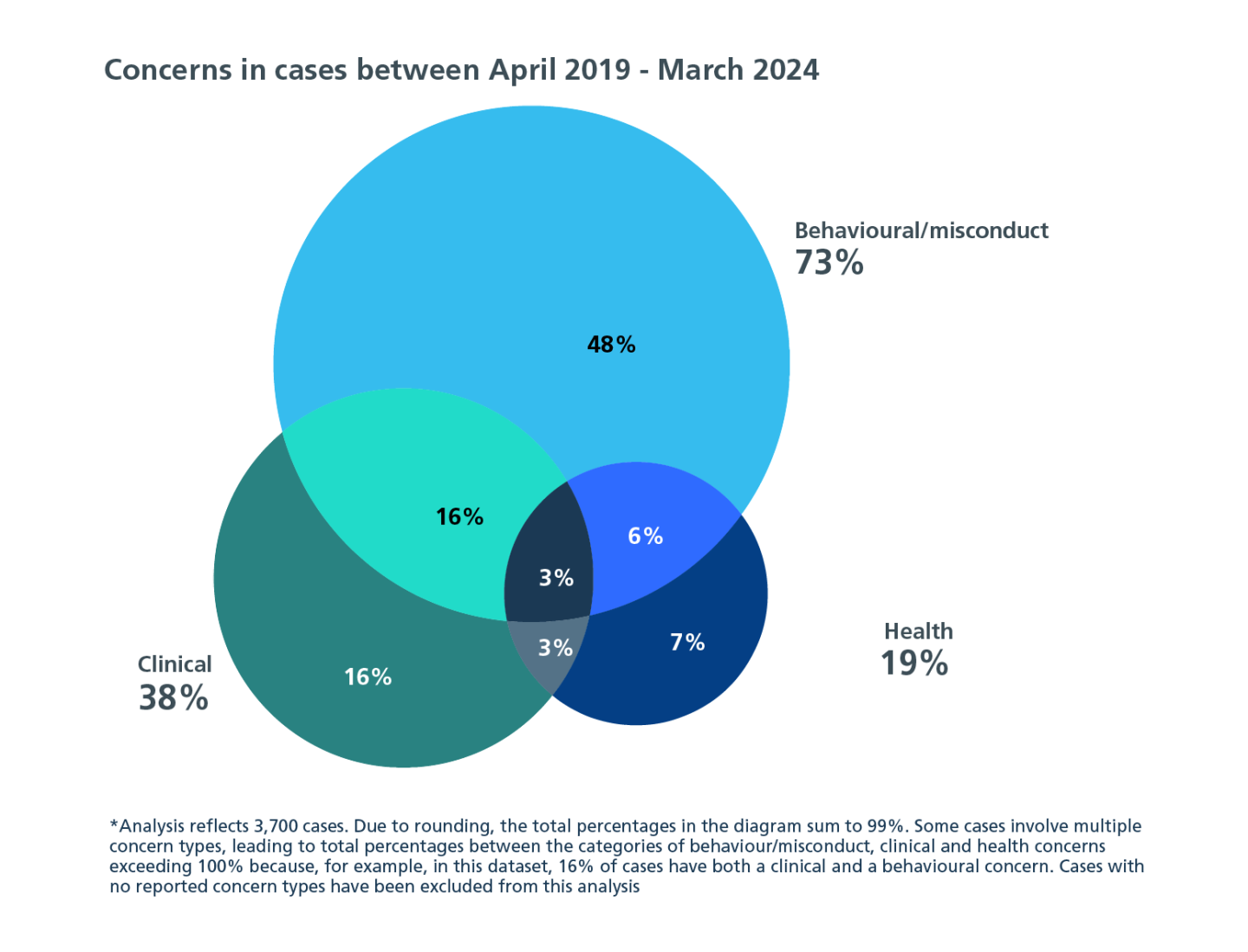
Seventy-three per cent of cases involved a behaviour/misconduct concern, which ranged from poor communication with colleagues, issues with teamwork and breaches of confidentiality, to incidents of theft or fraud. This has not changed substantially from our two previously published analyses of concerns, which found 70% of cases involved this type of concern.
You may find the resources below useful in gaining a better understanding of the behavioural concerns we see in our cases.
- Analysis of 141 of our behavioural assessments of doctors found an overarching theme of a lack of self-awareness and insight.
- Our recent Insight, Key themes, case studies and use of our services, analyses the concerns in our cases involving secondary care specialties and provides case studies that relate to behavioural, clinical, health and team working concerns, providing useful insights for managing concerns in any sector.
Professional groups
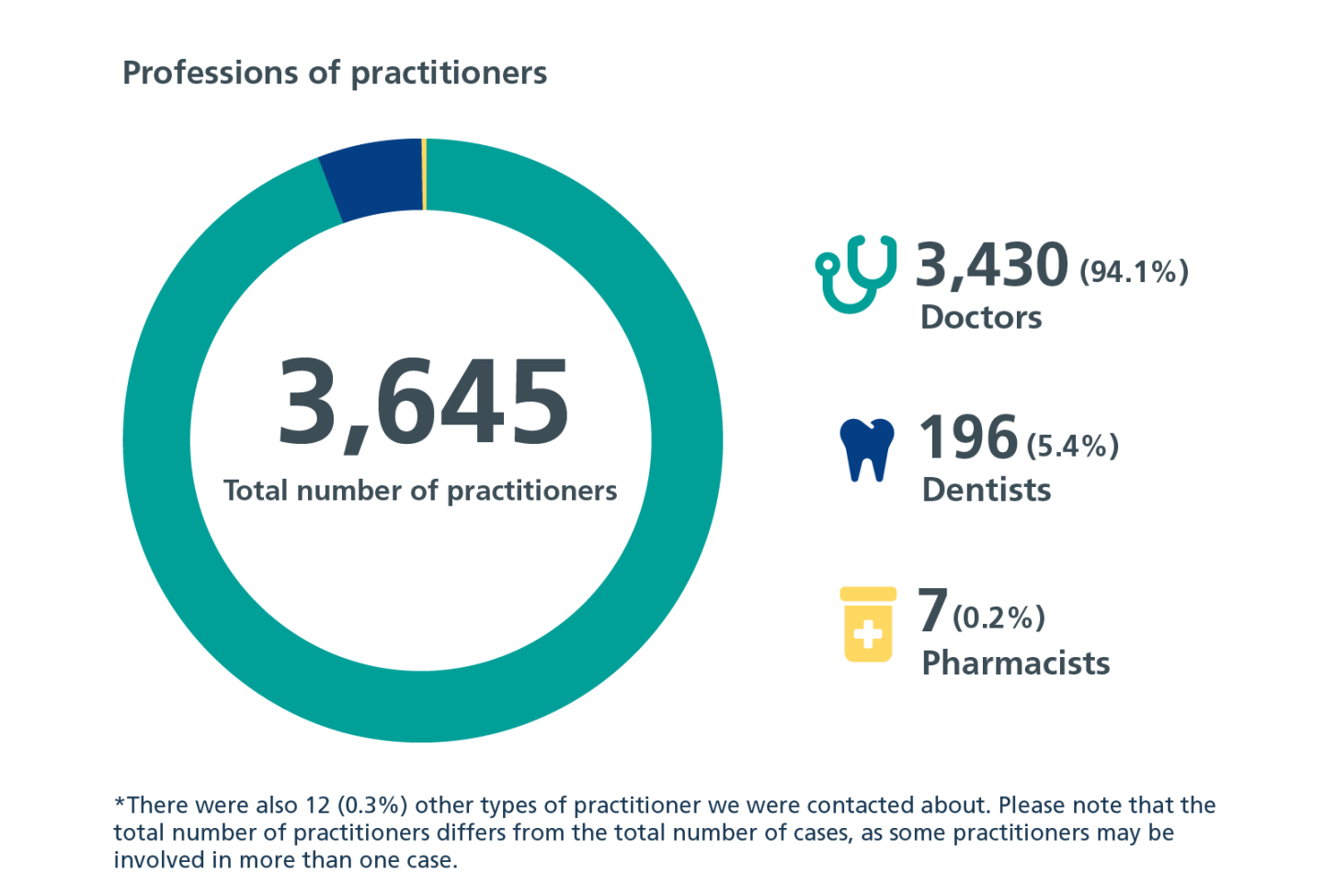
Between April 2019 and March 2024, our cases involved 3,645 practitioners with the highest number of cases about doctors, followed by dentists then pharmacists.
Practitioner demographics
We conducted an analysis of the personal characteristics of the practitioners in our cases against the NHS workforce of GPs, secondary care doctors and dentists in England1 and the General Medical Council (GMC) Medical Register data with the aim of understanding if any groups are overrepresented and, if so, to what extent.

Age and gender
We observed a higher case rate for male compared with female practitioners, making males 2.8 times more likely to have a case with Advice. In terms of age, the rate of cases for practitioners increased with each advancing age group. Practitioners who were aged 65 and over had 7.7 times the rate of cases per 1,000 than those aged under 35 years. Similarly, we have found that male doctors and dentists and those aged 65 and over are statistically more likely to be excluded2.
Ethnicity and place of qualification
Practitioners from ethnic minority groups had 1.3 times the rate of cases per 1,000 practitioners compared with white practitioners. Practitioners who qualified outside the UK had 1.6 times the rate of cases per 1,000 practitioners compared to those that qualified in the UK. We recognise that ethnic minority and IMG practitioners are disproportionately impacted by formal disciplinary processes as discussed in Fair to Refer published by the GMC3 and the NHS4. From research and analysis of Advice cases we have found that:
- Doctors and dentists who are statistically more likely to face exclusion are from Asian or Asian British, Mixed or from ‘Any Other Ethnic Group5.
- From research into the lived experience of ethnic minority and IMG practitioners with our service, there was a mixed picture in terms of whether practitioners felt they had been treated fairly by Advice and their employer; most participants described feeling discriminated against and long-term impacts included trauma, stress and anxiety6.
In response to the lived experience research, we produced an initial action plan which outlines a range of internal actions for Advice to take forward to help to improve the fairness and transparency of the service for all practitioners.
International medical graduates (IMGs) in Advice cases7
There is an increasing number of IMGs joining the workforce, lending further weight to the need to address the underlying causes of the higher proportions of IMG practitioners where concerns are raised about their practice. In 2022 more than half (52%) of the doctors who joined the workforce were IMGs and the number of IMGs joining the General Practitioner Register has almost tripled (+192%) from 2018 to 20228.
In the GMC’s recent report, Equality, diversity and inclusion: Targets, progress and priorities for 2024 9, they have said that “From the early days of education and training, to the leadership positions of latter years, issues of inequality are persistent and pernicious”. There are some early signs of progress, with the disparity in fitness to practise referrals in relation to a doctor’s ethnicity or place of qualification reducing.
‘Outsiders’ have poorer inductions, feedback and ongoing support, are more likely to work in isolated roles and are more vulnerable when things go wrong in cultures that focus on blame rather than learning.
IMG Advice cases: Grade groups in primary and secondary care
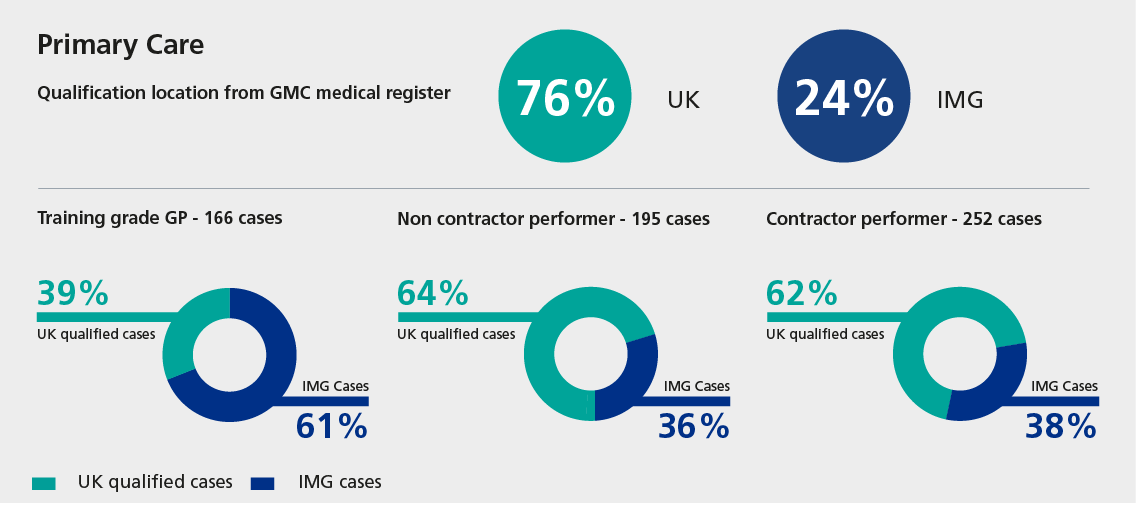
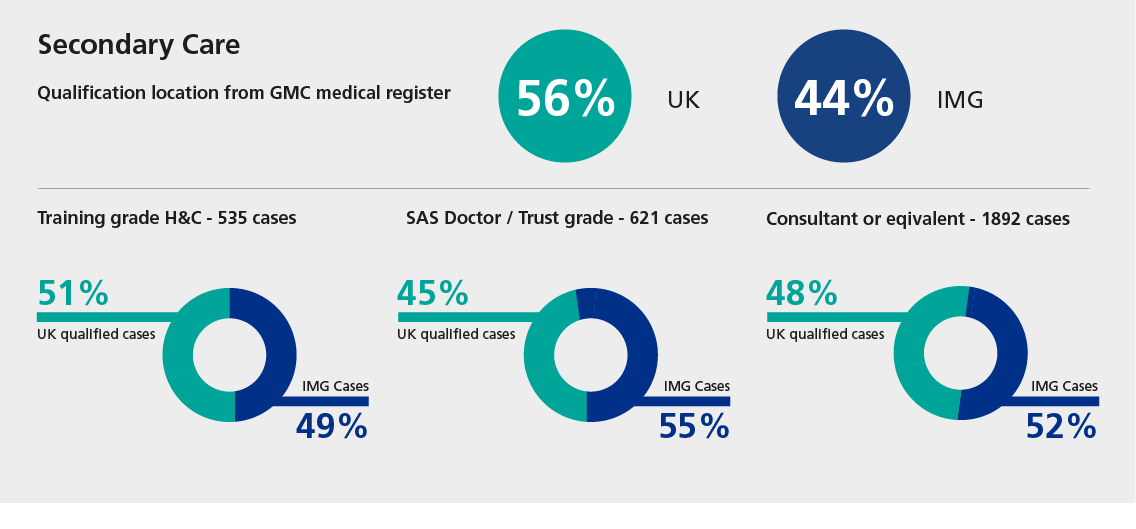
When examining our cases by place of qualification and grade group across primary and secondary care, we observed higher proportions of cases for IMGs (61%) who are training grade GPs. Even accounting for the increase in IMGs joining the General Practitioner Register, IMGs only accounted for 23% of those on this Register in 2023. Regarding secondary care, the proportions of Advice cases more closely reflect the workforce.
IMG Advice cases: Length of time in post
The GMC’s publication Fair to refer3 found that IMG doctors are impacted by insufficient inductions and lack of access to ‘the informal rules of the NHS’ and navigating the new social, cultural, and professional environment. More recent research into team working identified inclusivity and awareness of EDI issues as a key enabler of effective teamworking11.
We examined our cases by the length of time the practitioner was in post at the time the concern was brought to Advice. When considering the data below, please note that the post referred to will not always be the practitioner’s first post in the NHS. For cases where practitioners were in post for under one year, 70% were IMGs, and this fell to 43% of practitioners who had been in post for more than 10 years. It is not possible to state with certainty the causes of this from the data alone, but we recognise this is an area which would warrant further consideration with relevant stakeholders in the healthcare system, with a focus on induction and support required throughout the career of an IMG.
Note: Analysis reflects 3,234 cases involving doctors, dentists and pharmacists in England, Wales, Northern Ireland, and ‘other territories’. Due to changes in categories and the inability to completely map previous categories to new categories, some data has been excluded from this analysis.
What should healthcare organisations do next?
We invite healthcare organisations to consider the findings and how you engage with Advice with regards to the following:
- If you are interested in discussing your organisational activity report to reflect on themes and trends in your cases over time, please contact us at: nhsr.casesupport@nhs.net.
- Do you contact Advice early enough? Earlier involvement of Advice can lead to earlier resolution. There is no threshold for contacting Advice, nor any restriction to contacting Advice in only those cases where formal procedures are invoked. For more information on formal and informal case management, please see our Expert View Insight from Sally Pearson, our Responsible Officer and HPAN Lead at NHS Resolution.
- Could my organisation benefit from the just and learning culture charter at the end of Being fair 2 or our training courses to provide healthcare organisations with the knowledge and skills to identify and manage performance concerns locally?
Our Insights publications share analysis and research which draw on our in-depth experience providing expert, impartial advice and interventions to healthcare organisations. By sharing these Insights, we aim to support the healthcare system to better understand, manage and resolve concerns about doctors, dentists or pharmacists. You can find all past reports here.
If you are interested in hearing more about our research and Insights programme, please get in touch with us at nhsr.adviceresearchandevaluation@nhs.net or sign up to receive Insights by email.
If you’d like to learn more about our work and the services we offer, please visit our dedicated Practitioner Performance Advice webpages. Our Education service offers training courses to provide healthcare organisations with the knowledge and skills to identify and manage performance concerns locally.
Footnotes
1 There is no equivalent data for Wales and Northern Ireland to reproduce this analysis with these countries.
2 Exclusion trends and evaluation of NHS Resolution resources to manage exclusions (Practitioner Performance Advice, 2023).
3 Fair to Refer? (GMC, 2019).
4 Medical Workforce Race Equality Standard (MWRES) WRES indicators for the medical workforce 2020 (NHS England/Improvement, 2021).
5 Exclusion trends and evaluation of NHS Resolution resources to manage exclusions (Practitioner Performance Advice, 2023).
6 Experiences of ethnic minority and IMG practitioners: Research to improve fairness in the management of concerns (Practitioner Performance Advice, 2024).
7 The time period for the analysis in this section was April 2019 to mid March 2024 due to a change in our case management system.
8 The state of medical education and practice in the UK Workforce report 2023 (GMC).
9 Equality, diversity and inclusion: Targets, progress and priorities for 2024 (GMC).
10 Being fair 2: Promoting a person-centred workplace that is compassionate, safe and fair (NHS Resolution, 2023).
11 Teamworking: Understanding barriers and enablers to supportive teams in UK health systems (GMC, 2024).
Published:






